Antibiotic resistance is casting an increasingly long shadow over today’s healthcare landscape, undermining the ability to combat infections that were once readily manageable.
Among these, nontuberculous mycobacteria infections are notorious for their stubborn resistance to conventional medication and their penchant for afflicting those with existing lung diseases such as bronchiectasis, chronic obstructive pulmonary disease and cystic fibrosis.
The elderly and those with underlying conditions are particularly vulnerable, with the incidence of infection doubling in these demographics and contributing to a significant rise in public health costs.
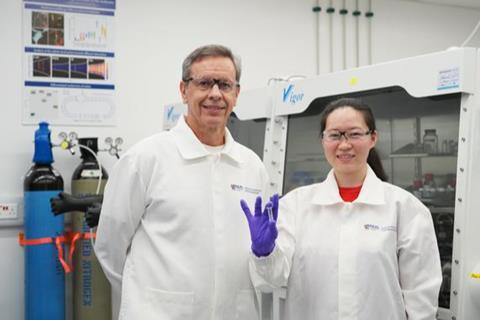
Researchers from the Institute for Functional Intelligent Materials (I-FIM) at the National University of Singapore (NUS) have innovated a conjugated oligoelectrolyte (COE)-based compound that has the potential to turn the tide on the disease. Called COE-PNH2, this novel agent not only demonstrates high efficacy against Mycobacterium abscessus (Mab), one of the most prevalent mycobacteria species, but also shows a blend of potency and safety that could reshape the treatment paradigm for persistent lung infections.
Interdisciplinary study
The researchers’ interdisciplinary study, partly funded by NUS Yong Loo Lin School of Medicine’s (NUS Medicine) Kickstart Initiative, was published in scientific journal Science Translational Medicine on 21 February 2024. Kickstart Initiative is a translational medicine programme aimed at bringing NUS Medicine’s promising biomedical research projects to market.
This study is led by Professor Guillermo Bazan, a principal investigator at I-FIM, and Department of Pharmacology at NUS Medicine, in collaboration with Associate Professor Kevin Pethe, Provost’s Chair in Infectious Disease, Nanyang Technological University, Singapore’s Lee Kong Chian School of Medicine (LKCMedicine).
Individuals afflicted with nontuberculous mycobacteria infections often stumble upon many hurdles when it comes to treatment. Regimens are arduous, cure rates are unsatisfactory, and side effects are difficult to bear. Even when the infection appears to be successfully reined in, the threat of relapse is not off the table.
Daunting challenges
Conventional antibiotics often falter — the bacteria’s uncharacteristically thick and impermeable cell envelope, as well as a shrewd evolutionary sleight of hand, have made the pathogens especially resistant towards common treatments. Additionally, the ability of the bacteria to enter a dormant state — forming what is referred to as persisters, poses a daunting challenge in antibiotic therapy, as these persisters often survive traditional treatments only to cause relapse.
Here is where COEs shake things up. A class of antimicrobial compounds with a modular molecular framework, COEs can be engineered into a panoply of therapeutic agents to fight a broad spectrum of infections. “COEs represent a fundamentally different approach to antibiotic design,” noted Prof Bazan, a corresponding author of the study. “Their unique structure, which facilitates the spontaneous interaction with lipid bilayers, allows them to breach the bacterial defences that so often thwart existing drugs.”
COE-PNH2, the molecule designed and crafted by the I-FIM researchers, is optimised to target Mab, employing a dual mechanism that disrupts the bacterial membrane and obstructs vital bioenergetic pathways — a one-two punch that leaves the bacteria with little room to hide. In particular, the molecule attacks both replicating and dormant forms of Mab, exhibiting robust bactericidal activity that leads to a more comprehensive eradication of the bacteria, leaving no refuge for resistance to crop up while reducing the likelihood of relapse.
Achilles heel
“Resistance development is often the Achilles’ heel of new antibiotics,” said Prof Bazan. “COE-PNH2 exhibited a low frequency of resistance in our study, which suggests that it may remain effective longer than existing treatments, providing patients with a more durable solution.”
Safety is also a cornerstone of the new antibiotic. It demonstrated low toxicity in mammalian cells and did not induce the destruction of red blood cells (haemolysis) at concentrations far exceeding those required for antibacterial activity. This noncytotoxic nature underscores COE-PNH2’s potential as a therapeutic agent with a wide margin of safety.
This safety is also reinforced through in vivo studies. When tested in a preclinical model of acute lung infection, the novel compound was well-tolerated, while its therapeutic effect was pronounced, achieving a substantial reduction in bacterial load without the emergence of resistant strains.
Path to clinical use
“As COE is a relatively new antibiotic platform, the subsequent phase of this study requires us to understand the mechanism of action of the drug in greater detail,” highlighted corresponding author of the study Assoc Prof Pethe, noting that moving the novel compound along its journey from petri dish and in vivo studies to patient is very much a work in progress.
For starters, unravelling the molecular interaction between COE-PNH2 and mammalian and bacterial cell membranes is crucial. Furthermore, there is a need to dissect various mechanisms through which the compound functions. For instance, it is unclear to the researchers whether the hydrogen-bonding moieties of the compound contribute to its enhanced potency against nutrient-starved persisters. Uncovering the precise manner in which COE-PNH2 compromises these resilient forms could shine new light on more effective strategies for combating dormant bacterial strains.
Intracellular vesicles
Intriguingly, the researchers have also discovered the presence of intracellular vesicles in Mab treated with COE-PNH2. Are these vesicles by-products of disrupted bioenergetics, or do they form as a result of physical interactions between the compound and the membrane lipids? The answers may provide vital insights into how COE-PNH2 exerts its antimicrobial action and inform the development of interventions for other hard-to-treat pathogens.
“Mycobacterium abscessus infections are notoriously difficult to treat as the organism is resistant to multiple classes of antibiotics, hence a new class of antibiotics will add to our armamentarium to fight the infection,” said Dr Catherine Ong, Senior Consultant at the Division of Infectious Diseases, Department of Medicine, National University Hospital.
The combined efforts by researchers at I-FIM, NUS Medicine, and LKCMedicine is one step in the right direction where a range of microbial maladies can be dealt with by harnessing the therapeutic potential of COEs.
Topics
- Antimicrobial Resistance
- Antimicrobials
- Asia & Oceania
- Bacteria
- Catherine Ong
- COE-PNH2
- conjugated oligoelectrolytes
- Guillermo Bazan
- Infection Prevention & Control
- Infectious Disease
- intracellular vesicles
- Kevin Pethe
- Nanyang Technological University
- National University of Singapore
- Non-tuberculous mycobacterium
- Pharmaceutical Microbiology
- Research News






No comments yet