New research has revealed the mechanism of transcriptional regulation via S-nitrosylation for resistance to last resort drug vancomycin in Staphylococcus aureus.
A research team led by Prof. Sun Baolin from the University of Science and Technology of China (USTC) outlined the work in a paper published in Nature Communications.
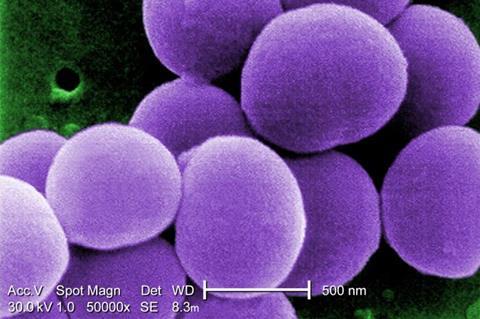
Staphylococcus aureus is a major human pathogen, and infections caused by methicillin-resistant S. aureus (MRSA) are posing serious threats to public health. Vancomycin is considered to be a last-resort drug in the treatment of severe MRSA infections, but the frequent emergence of vancomycin-intermediate S.aureus (VISA) brings a great challenge.
Nitric oxide (NO), a signaling molecule, was first discovered to be endogenously generated by nitric oxide synthase (NOS) in eukaryotes and is involved in regulating various physiological and immune functions. Previous researches have reported that NO can mediate the S-nitrosylation modifications of cysteine residue, consequently affecting the activity and functions of protein. Researchers have verified that NOS exists in S. aureus and is involved in regulating the vancomycin resistance, but the molecular mechanism remains unclear.
Uncovering the mechanism
To reveal the mechanism, researchers first constructed NOS mutant strain and add NOS inhibitor exogenously in a clinically isolated VISA strain XN108. Then, proteomic analysis identified the target protein and corresponding sites that can be modified by NO-mediated S-nitrosylation in S. aureus.
MgrA, a transcription regulator involved in antibiotics resistance, was found to be S-nitrosylated at cysteine residue Cys12. Researchers generated the mgrAC12S mutant strain by replacing the Cys12 with a serine, which can’t be S-nitrosylated. The mgrAC12S mutant strain showed a significant decrease in vancomycin resistance and cell wall thickness as well as an increase in autolytic activity.
The team used methods like fluorescent quantitative PCR, gel-shift experiment and chromatin immunoprecipitation assay to reveal the roles of S. aureus NOS and the endogenously generated NO in promoting vancomycin resistance. NO generated by NOS mediates the S-nitrosylation of MgrA, which negatively regulated autolysis in S. aureus, causing an increase in cell wall thickness thereby promoting the vancomycin resistance.
Such NO-mediated regulation mechanism was further verified in another transcription regulator WalR that can be modified by S-nitrosylation, indicating that this mechanism could be universal in bacteria.
This study is expected to provide new ideas and strategies for the clinical treatment of VISA and other bacterial pathogen infections.






No comments yet