The anthrax outbreak in Africa could be a harbinger of more to come, with climate change creating opportunities for the emergence of more cross-over strains capable of causing anthrax-like infections.
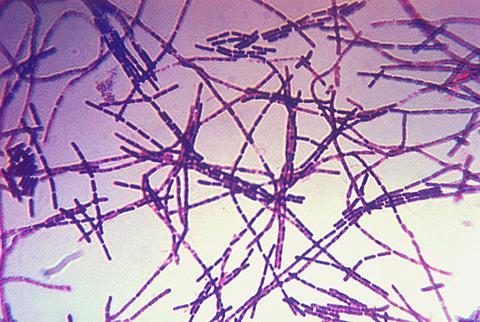
The recent outbreak of anthrax in Africa has yet again focused attention on this notorious pathogen. It is caused by the spore-forming bacterium Bacillus anthracis, a member of the Bacillus cereus group which includes several closely related species.
Differentiating B. anthracis from other members is complicated by the ability to transfer the pathogen’s plasmid-borne virulence factors, a tripartite toxin (pXO1) and a protein-based anti-phagocytic capsule (pXO2), between species.
This has led to the emergence of ‘new’ pathogenic variants, such as the recently described B. cereus var anthracis, which possess homologs of the pXO1 and pXO2 plasmids and has been isolated from elephants, goats and non-human primates in West and Central Africa.
Domestic livestock
While primates such as humans are susceptible to infection from wildtype B. anthracis, it primarily affects domestic livestock such as cattle, sheep and goats, as well as wild herbivores such as deer and hippopotami.
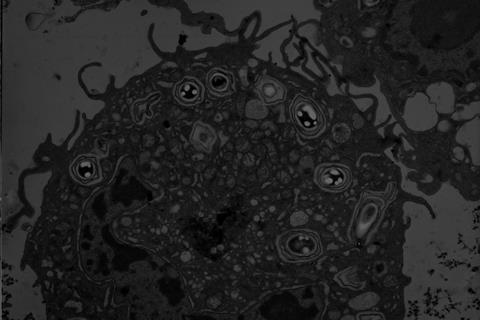
Death is often sudden and is due to a combination of massive bacteraemia and toxin production. Upon death, the vegetative form of the bacterium converts into an inert spore which allows the organism to survive in the environment until it encounters a new host. These prolonged periods of dormancy probably account for the high levels of genetic conservation observed in all isolates of this species encountered to date.
Studies suggest that limited replication can occur outside of a host provided the environment is permissive. Factors identified as being important include calcium and organic-rich soil, a pH above 6.0, ambient temperatures above 15.5°C, vegetation coverage and water content.
Mystery of infection
The mechanism by which B. anthracis spores in soil infect susceptible animals is unclear. It may be the case that herbivores are exposed to spores associated with certain grasses. The ability of B. anthracis spores to replicate and exchange genetic material in the rhizosphere of grass plants has been reported.
Thus, as global temperatures rise, more opportunities may arise for the pathogen to replicate and pass on its virulence genes to other members of the B. cereus group. Field studies have also confirmed the ability of B. anthracis to promote plant growth and it has been proposed that this mechanism attracts susceptible grazing animals to spore-contaminated locations.
Heat and flooding
Another possibility is that flooding results in the mechanical transport of spores to local watering holes, where the concentration is sufficient to infect animals. The infective process may also be facilitated by periods of summer heat which generate spore-contaminated dust and reduce the resistance of susceptible animals to airborne infection. Flies are also thought to play a role in the spread of spores and infection of new hosts.
Infection in humans is normally the result of exposure to contaminated animals or their products. The first human cases of the current outbreak occurred in Zambia in May 2023. Further cases were linked to the consumption of meat from the carcasses of wild hippopotami who had died of unknown causes.
The spread of infection to neighbouring countries has been linked to limited community knowledge regarding anthrax transmission, unrestricted cross-border movement of infected animals and carcasses, poverty and food insecurity and a shortage of available vaccines. To this point, the Zambian Ministry of Health acknowledged the complete lack of anthrax vaccines in country in a recent press statement.
Climate change
It has been suggested that climate change may have exacerbated the problem. Evidence in support of this hypothesis comes from an outbreak of anthrax in reindeer which occurred in northern Russia in 2016. Anthrax killed thousands of animals and affected dozens of humans on the Yamal peninsula, in Northwest Siberia.
Two primary factors have been identified as contributing to this outbreak, a summer heat wave which caused the permafrost to melt releasing ‘trapped spores’ and the cancellation of the reindeer vaccination programme in 2007 which led to an increase in population susceptibility. Using a machine-learning approach based on reported anthrax outbreaks in the northern latitudes, Walsh and colleagues predict an increase in future anthrax outbreaks as a consequence of an increase in mean global temperatures.
In conclusion, outbreaks of anthrax in endemic regions of the world are not unusual. We are likely to see more cases due to a combination of climate change and socio-economic factors, such as food poverty and lack of access to effective veterinary services.
Increased cases in more prosperous northern latitudes may also occur but will be limited by access to healthcare and veterinary services. Changes in the climate could create opportunities for the emergence of more cross-over strains capable of causing anthrax-like infections.
Article courtesy of Les Baillie and Alexandra Cusmano, School of Pharmacy and Pharmaceutical Sciences, Cardiff University, King Edward VII Avenue, Cardiff CF103NB. Bailliel@cardiff.ac.uk
Topics
- anthrax
- Applied Microbiology International
- Artificial Intelligence & Machine Learning
- Asia & Oceania
- B. cereus var anthracis
- Bacillus anthracis
- Bacillus cereus
- Bacteria
- Climate Action
- Community
- dormancy
- Economic Equality
- Infectious Disease
- Middle East & Africa
- Northwest Siberia
- One Health
- plasmids
- pXO1
- pXO2
- rhizosphere
- spores
- Veterinary Medicine & Zoonoses
- virulence factors
- Zambian Ministry of Health







No comments yet