The Hepatitis B virus is a leading cause of liver-related morbidity and mortality, particularly through chronic hepatitis B (CHB), which can progress to cirrhosis and liver cancer. While most adults recover from acute hepatitis B (AHB), a significant proportion of infants and children develop chronic infections. Despite advancements in treatment, an effective cure for chronic HBV remains elusive.
A new study explored the immune dynamics across different phases of HBV infection, including acute hepatitis B, immune tolerance, immune activation, and inactive chronic infection, using single-cell RNA and TCR/BCR sequencing.
READ MORE: Hepatitis B: new rapid diagnostic test to halt mother-to-child transmission
READ MORE: Digging into a decades-old hepatitis B mystery suggests a new potential treatment
By analyzing liver and paired blood samples from 18 patients in various infection phases, along with healthy controls, the study provides new insights into immune transitions during HBV infection.
Key findings
Intrahepatic T Lymphocytes: Three distinct types of blood-derived intrahepatic T cells (hpCTLs) were identified: exhausted, short-lived effector, and GZMB+ CTLs. Key factors such as FasL/Fas, CD28 co-stimulation, and T cell exhaustion play critical roles in T cell function during HBV clearance.
DC-SIGN+ Macrophages: These liver-resident macrophages were found to have dual roles—serving as antigen-presenting cells to activate T cells while simultaneously suppressing T cell immunity through IL-10 and PD-L1, as well as promoting Treg cell recruitment.
Hepatocyte Subsets: The Hep1 hepatocytes around the central vein and Hep2 hepatocytes around the portal vein exhibit different sensitivities to HBV infection and innate immune responses. Liver priming and insufficient IL-2 signaling may be associated with T-cell dysfunction during the IT phase.
Dynamic immune phenotypes
Immune characteristics in the IA phase: DC-SIGN+ macrophages, along with CSF1+ST2+ mast cells, IL-33+ liver sinusoidal endothelial cells, and Treg cells, collectively create a type 2 immune suppressive environment in the liver during the IA phase. Furthermore, the IA phase is characterized by an enhanced humoral immune response, including an upregulation of plasma cells and IgG1.
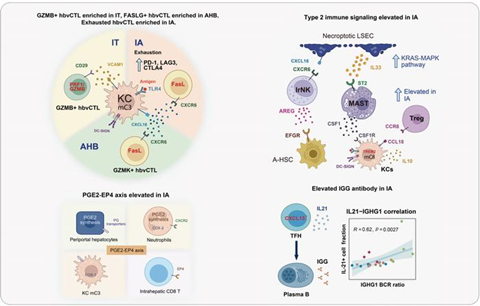
Overall, the study reveals dynamic immune phenotypes in the progression of HBV infection. It provides valuable insights into the molecular mechanisms that drive immune suppression and activation, identifying potential new targets for immunomodulatory therapies to treat chronic hepatitis B. The research team from the School of Life Science and Technology at Harbin Institute of Technology hopes that these findings will contribute to the development of more effective therapeutic strategies for chronic hepatitis B. The PhD student, Chuangeng Chen, from Harbin Institute of Technology is the first author of this work.

No comments yet