A CABI-led study published in the CABI Agriculture and Bioscience journal has revealed “considerable farmer knowledge” on different aspects of antibiotics risks – including antimicrobial resistance – associated with their use on livestock in Kenya.

Scientists from CABI’s regional centre for Africa in Nairobi, Kenya, joined colleagues from the University of Nairobi, the University of Warwick, UK, and VSF Suisse, to carry out the research where Kenya is an antimicrobial resistance (AMR) hotspot.
The researchers conducted a survey among 319 farming households in five counties in Kenya and found that 19 of 21 knowledge statements on AMR and safe use of antibiotics were answered correctly by 55-89% of respondents. This indicates, they say, considerable farmer knowledge on different aspects of antibiotics risk.
Threat to treatment
The researchers say that while the number of livestock owned was the factor most positively influencing farmers’ knowledge on AMR and safe use of antibiotics,
Certain knowledge gaps remain, and their “practices continue to constitute considerable risk of further AMR development.”
Mr Harrison Rware, lead author on the study, said, “This study assesses farmers’ knowledge and practices on antibiotics in livestock production, knowledge on AMR as well as factors influencing farmers’ knowledge of antibiotic safety and resistance, and antibiotics use.
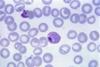
“Antibiotics have been frequently utilized in this context to reduce the spread of numerous cattle diseases and increase. However, the use of antibiotics in livestock has sparked public debate globally, primarily due to concerns about inappropriate use and the associated risk of antimicrobial resistance.
“AMR poses a significant threat to effective infection treatment, in humans and animals, leading to increased morbidity and mortality rates, as well as escalated healthcare cost.”
Majority buy antibiotics without prescription
Around 80% of households surveyed use antibiotics in their livestock, and 58% administer the antibiotics themselves – the vast majority of which buy antibiotics without a prescription, the researchers found.
They add that antibiotics are used for both therapeutic and non-therapeutic purposes, the latter in the form of growth promoters and feed enhancers in poultry.
Meanwhile, the withdrawal periods reported by farmers are shorter than the officially recommended periods. Although many farmers reported risky antibiotic practices, most (76%) were aware of bacterial AMR.
Mr Rware added, “Kenya has made notable progress towards creating knowledge and awareness of farming communities on the risks and requirements associated with antibiotic use in livestock.
“Nonetheless, farmers’ antibiotics practices continue to constitute considerable risk of further AMR development. This shows that knowledge is not enough to ensure fundamental behavioural change.”
Enabling environment
He said there needs to be an enabling environment driven by effective policy interventions and enforcement to ensure compliance with set guidelines for antibiotic use as well as research on and deployment of alternatives, such as probiotics, vaccinations, and disease prevention measures.
“There also needs to be continued public awareness raising and education using multiple channels to reach farmers and strengthen cross-sector, multi-stakeholder collaboration to address the multi-national complexities of AMR.”
Further research into farmers’ perceptions and decision-making processes, as well as systems’ factors preventing farmers from adopting safer practices, the researchers conclude, will yield insights into the drivers behind risky practices and required solutions.





No comments yet