Inflammatory bowel disease (IBD) is characterized by chronic inflammation of the gastrointestinal tract and is primarily referred to as ulcerative colitis and Crohn’s disease. As the number of patients suffering from IBD increases, diagnosis and treatment have become pressing yet challenging tasks.
A major challenge is that patients with IBD do not exhibit characteristic symptoms, making it difficult to differentiate between IBD and other intestinal abnormalities. Endoscopy is the most conventional method used to diagnose IBD; however, this method is invasive and expensive.
Therefore, affordable non-invasive techniques need to be developed for diagnosing IBD, highlighting the need to identify biomarkers specific to the disease.
It is now established that the gut microbiome contributes significantly in the development of IBD, and changes in the abundance of various organisms in the gut have been widely explored to identify microbial signatures associated with IBD.
Biomarkers and IBD
A new review discusses the current state of knowledge on biomarkers in IBD, with a primary focus on the gut microbiome, associated metabolic signatures, and their links with immunological biomarkers. These biomarkers can help propose an integrative model to better understand the pathophysiology of this complex disease. This integrated approach will also provide insights into potential therapeutic targets for designing appropriate treatment strategies for patients.
The global prevalence of IBD has surged, with 4.9 million cases reported in 2019, driven by environmental, genetic, and lifestyle factors. Incidence rates for CD and UC have risen dramatically, with higher morbidity in older adults and individuals with familial predispositions. The economic burden is significant, particularly in regions like Europe and Iran, where treatment costs vary by disease severity and healthcare systems.
Factors affecting IBD
IBD etiology involves a complex interplay of genetic susceptibility (e.g., HLA gene variants), environmental triggers (e.g., diet), and microbial dysbiosis. Polymorphisms in immune-related genes, such as TNFα and IL-1, exacerbate inflammation, while diet shapes microbiome composition. Notably, the NOD2 gene variant correlates with Enterobacteriaceae abundance, linking genetics to microbial imbalance.
The gut microbiome in IBD patients exhibits reduced alpha diversity and altered composition, marked by:
Bacteria: Decreased F. prausnitzii (butyrate producer) and increased Enterobacteriaceae (e.g., E. coli), contributing to inflammation.
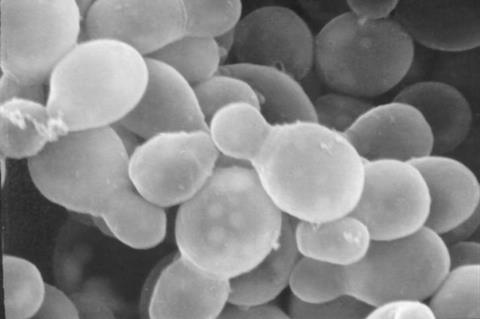
Fungi: Elevated Candida albicans and Malassezia, which promote pro-inflammatory cytokines like IL-17.
Viruses: Enriched Caudovirales phages, associated with bacterial dysbiosis. Extracellular vesicles (EVs) from gut microbiota and host cells modulate immune responses and serve as potential biomarkers, with miRNAs and proteins like ANXA1 linked to disease activity.
Metabolome signatures in IBD
Dysbiosis disrupts metabolite profiles, including:
-
Short-chain fatty acids (SCFAs): Reduced butyrate levels impair anti-inflammatory responses.
-
Bile acids and TCA cycle intermediates: Altered in IBD, correlating with disease severity.
Metabolomic techniques (NMR, MS) reveal distinct fecal and serum profiles, aiding in differentiating CD from UC and predicting treatment responses.
Immunological Biomarkers
Key immune markers include:
-
Diagnosis: Anti-Saccharomyces cerevisiae antibodies (CD) and pANCA (UC).
-
Prognosis: Oncostatin M (OSM) predicts non-response to anti-TNF therapy.
-
Treatment Monitoring: Elevated IL-1β, IL-8, and CXCL chemokines during relapse.
Dysbiosis-driven metabolite changes (e.g., low SCFAs) exacerbate inflammation via NF-κB and NLRP3 pathways.
Integration of Biomarkers
An integrative model links microbiome shifts (e.g., F. prausnitzii decline) to reduced butyrate, disrupting Th17/Treg balance and elevating IL-6/IL-17. Such interactions highlight the potential for multi-omics approaches to unravel IBD mechanisms.
Machine learning algorithms analyze microbiome and metabolome data to predict disease flares and therapy responses. Challenges include dataset diversity and model generalizability, but AI holds promise for personalized IBD management.
Longitudinal studies and multi-omics integration are needed to validate biomarkers across diverse populations. Research should explore causal microbiome-immune relationships and therapeutic microbiome modulation.
This review underscores the interconnected roles of microbial, metabolic, and immune biomarkers in IBD. While current biomarkers lack universal specificity, integrative approaches and AI-driven analyses offer transformative potential for precision medicine in IBD care.







No comments yet