Transferring the mother’s vaginal bacteria onto newborns delivered via Caesarean section appears to be beneficial to infants’ early development, researchers have reported.

Reported in the journal Cell Host & Microbe, the study, the first triple-blind experiment of its kind, suggests a potential approach to improve the early gut microbiota of babies born through C-section.
Infants born by C-sections tend to have very different gut bacteria composition compared with those born vaginally, according to previous research.
Early gut bacteria
Vaginally born babies receive their early gut bacteria from the mother’s birth canal, while C-section babies’ microbiota are dominated by bacteria found on the mothers’ skin, in breastmilk, and in the environment. While the difference tends to disappear as they age, researchers suggest early gut microbiota is associated with the development of an infant’s immune system and could affect their disease risk, including for diabetes, later in life.
This has led to practices like vaginal seeding where mothers would rub C-section newborns with their vaginal fluids. But there is limited clinical evidence that vaginal seeding is safe and effective, says Yan He, the paper’s corresponding author at Southern Medical University in Guangzhou, China.
“When we talk about effectiveness, we not only mean whether this intervention might affect the infants’ microbiota but are also interested to see if this intervention could actually improve the infants’ phenotypes, like their neurodevelopment.”
C-section deliveries
To investigate whether vaginal microbiota seeding works, He and his team rubbed the lips, skin, and hands of 32 newborns delivered via C-section with a gauze soaked with their mothers’ vaginal fluids and another 36 newborns with a gauze soaked with saline as blind controls. The mothers were tested in advance to make sure they were free of infections such as sexually transmitted diseases and group B streptococcus.
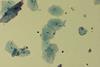
The team found that newborns who received the microbiota had more gut bacteria found in maternal vaginal fluid 6 weeks after birth, suggesting that maternal vaginal bacteria successfully reached and colonized babies’ guts.
Compared with C-section newborns who received saline gauze, babies with microbial transfer had more mature bacteria in their guts at 6 weeks old, similar to babies born vaginally. No infants experienced severe adverse events during the experiment.
Evaluating neurodevelopment
The team also evaluated the babies’ neurodevelopment at 3 months and 6 months after birth using a questionnaire. For example, the researchers would ask the mothers if their babies were able to make simple sounds or perform movements like crawling on their hands and knees.
The team found infants who received the seeding scored significantly higher in neurodevelopment at both 3 months and 6 months, and their scores were comparable to those of vaginally born babies.
“We don’t know exactly how early gut bacteria affect their neurodevelopment, but there is some indirect evidence that shows some microbial metabolites are related to conditions,” he says.
Increased metabolites
For example, the team found that babies who received vaginal microbiota seeding had more indolelactic acid, a type of metabolite of several Clostridium bacteria species, in their faeces. Previous research has discovered that indolelactic acid levels are low in people with Parkinson’s disease and Alzheimer’s disease.
“We’re hoping this study can provide some leads to future research in this field. We want to know if vaginal microbiota seeding has the potential to reduce the risk of neurodevelopmental disorders in children, such as ADHD, ASD, and intellectual disabilities,” he says, adding that he and his team plan to carry out long-term clinical trials with larger sample sizes.
“It is somewhat like faecal microbiota transplantation. We need more data to understand this intervention and make it more precise. We may eventually uncover what exactly is beneficial in maternal vaginal microbiota, which could enable us to design therapeutics for all infants born via C-section in the future,” He says.
This work was supported by the National Key R&D Program of China, Canadian Institute of Health Research, National Natural Science Foundation of China, Clinical Research Startup Program of Southern Medical University, and the Top Talent Program of Affiliated Foshan Maternity & Child Healthcare Hospital.
Topics
- Affiliated Foshan Maternity & Child Healthcare Hospital
- Asia & Oceania
- Canadian Institute of Health Research
- Clostridium
- C-section
- Human Microbiome
- indolelactic acid
- National Key R&D Program of China
- National Natural Science Foundation of China
- neurodevelopment
- newborn babies
- One Health
- Reproductive &Urinary Tract Microbiome
- Research News
- Southern Medical University
- vaginal microbiome
- vaginal seeding
- Yan He






No comments yet