Despite progress in combating antimicrobial resistance (AMR) in the USA since its peak during the COVID-19 pandemic, hospital-acquired AMR infections remain well above pre-pandemic levels, according to a major new study examining AMR before, during, and after the COVID-19 pandemic in 120 US hospitals.
The study was led by Dr Christina Yek from the US National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health (NIH), and is being presented at this year’s ESCMID Global Congress (formerly ECCMID) in Barcelona, Spain (27-30 April). It reveals that AMR rates remain high largely due to the persistence of hospital-onset infections, in particular those caused by gram-negative resistant organisms.
These findings highlight the urgent need for action to identify the drivers of, and solutions for, difficult-to-treat gram-negative AMR.
Alarming rises
AMR is estimated to cause at least 35,000 deaths annually in the US and 1.27 million worldwide. In 2022, a US Centers for Disease Control and Prevention report described alarming rises in AMR across US hospitals during the first year of the COVID-19 pandemic, with resistant hospital-related infections growing 15% between 2019 and 2020. However, the key drivers and lasting effects of this phenomenon remain unexplored.
To provide an updated report on the status of AMR in US hospitals, researchers analysed trends in incidence of AMR infections in adults (aged 18 years and older) in 120 hospitals before (Jan 2018–Dec 2019), during (March 2020–Feb 2022), and after the pandemic (March–Dec 2022), that were continuously reporting in the PINC-AI database—an administrative dataset representing 20% of US hospitalisations.
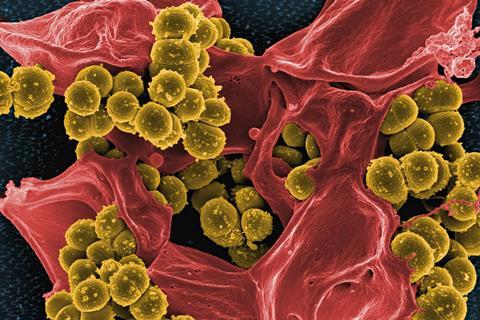
All hospitalisations were examined for culture-confirmed infection by six pathogens—methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococcus (VRE), extended-spectrum cephalosporin-resistant Enterobacterales (ECR), and carbapenem-resistant Enterobacterales (CRE), Acinetobacter baumannii (CRAB), and Pseudomonas aeruginosa (CR-PA)—acquired either before (community-acquired) or after three days of hospitalisation.
Hospiral-acquired infections
During the pandemic, the overall prevalence of AMR infections increased by 6.3% (from 181.9 to 193.3 per 10,000 hospitalisations; see figure 1 in notes to editors). This was driven primarily by a steep rise in hospital-acquired resistant infections, which rose at least 32% (from 28.7 to 38.0 per 10,000 hospitalizations), compared with community-acquired infections, which increased just 1.4% (153.2 to 155.3 per 10,000 hospitalizations).
During the pandemic, infections due to gram-negative pathogens—those that are resistant to multiple drugs and are increasingly resistant to most available antibiotics—increased by almost 20% compared to pre-pandemic levels, while resistant gram-positive infections fell by 4.2%.
The greatest increases were seen in hospital-acquired infections resistant to commonly prescribed antibiotics called carbapenems, which are considered the drugs of last resort for treating severe infections. These included infections caused by CRAB which grew 151% during the two years of the pandemic (0.5 to 1.3 per 10,000 hospitalisations), followed by CRE which rose 62% (1.1 to 1.8 per 10,000 hospitalisations), and CR-PA which increased by 54% (2.2 to 3.4 per 10,000 hospitalisations; see figure 2 in notes to editors).
Decreasing trend
In contrast, during and after the pandemic, community-acquired MRSA infections declined by 10% (from 71.1 to 63.7 per 10,000 hospitalisations) and 19% (71.1 to 57.8 per 10,000 hospitalisations), respectively. This decreasing trend, which had preceded the pandemic, may have been further boosted by reduced societal mobility and interactions as a result of pandemic restrictions.
Interestingly, the researchers also found that hospitals with the highest levels of surges in severely ill COVID-19 patients during the pandemic had the largest increases in hospital-acquired AMR infections, with incidence increasing in a stepwise fashion. Larger hospitals with the highest bed capacity (500 beds) had more than double the odds of AMR infections compared to hospitals with the lowest bed capacity (0-99 beds).
“It is likely that surges in severely ill COVID-19 patients during the pandemic corresponded with significant surges in antibiotic use and challenges following infection and prevention control protocols in strained hospitals,” says Dr Yek. “In addition, hospitals may have experienced shortages of personal protective equipment, while treating sicker patients who were more likely to require the use of medical devices like ventilators, which would have added to the spread of antimicrobial-resistant infections.”
US healthcare facilities
Post pandemic, overall AMR incidence has nearly returned to pre-pandemic rates (181.9 to 182.2 per 10,000 hospitalisations). However, hospital-acquired AMR infections remained 13% above pre-pandemic levels in December 2022 (28.7 to 32.3 per 10,000 hospitalisations), largely due to the persistence of gram-negative pathogen infections that are resistant to most available first-line antibiotics.
Between March and December 2022, infections due to hospital-acquired carbapenem-resistant organisms remained at least 35% higher than pre-pandemic levels—CRAB (up 43%), CRE (81% increase), and PR-PA (up 38%; see figure 2 in notes to editors).
“While overall antimicrobial resistance levels appear to have almost returned to pre-pandemic levels, the persistence of high rates of hospital-acquired AMR infections in US healthcare facilities is concerning. More action is needed to protect people, especially from difficult-to-treat hospital-acquired gram-negative infections that remain concerningly high,” says Dr Yek.







No comments yet