Researchers at The University of Texas MD Anderson Cancer Center have discovered that lactate-producing intratumoral bacteria drives resistance to radiation therapy, suggesting that lactic acid-producing bacteria present in various cancers may serve as novel therapeutic targets.
The study, published in Cancer Cell, reported that a particular bacterial species, Lactobacillus iners (L. iners), caused cancer cells to respond to radiation by rewiring metabolic signaling pathways to resist treatment. The researchers also found that L. iners was associated with poorer clinical outcomes in patients with cervical cancer.
“These lactic acid-producing bacteria are seemingly responsible for changing signaling pathways by priming cancer cells to use lactate instead of glucose to fuel growth and proliferation from oxidative stress following radiation therapy,” said corresponding author Lauren Colbert, M.D., assistant professor of Radiation Oncology. “This is potentially paradigm shifting, and we currently are working on novel approaches to target these specific intratumoral bacteria. We are hopeful that these efforts will lead us to approaches that can benefit patients across several types of cancer.”
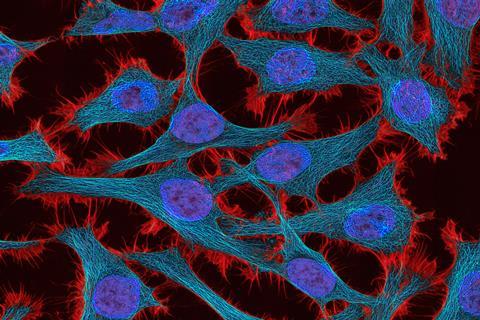
Tumor microbiome
Cervical cancer is a human papillomavirus (HPV)-related cancer that originates in the same way and is similar microscopically and genomically to anal and head and neck cancer. These types of cancers are commonly treated with different amounts of radiation.
Cervical cancers often respond well to treatment, but some patients develop resistance, leading Colbert and her colleagues to examine the role of the tumor microbiome in driving differential responses. Researchers used microbiome sequencing, targeting bacterial cultures and in vitro models to study the tumor microbiome in this context.
Cervical cancer offers an opportunity for easier repeated tumor microbiome sampling, allowing the researchers to perform large-scale sequencing analyses and targeted culture of tumor-resident bacteria from 101 patients with cervical cancer undergoing chemoradiation between September 2015 and March 2022.
They discovered that L. iners was associated with poor response to radiation and with decreased recurrence-free survival (RFS) and overall survival (OS), even when accounting for known clinical risk factors, gut microbiome factors and immune environment factors in the tumor and in patients’ blood. This led the researchers to also perform targeted culture of this specific bacteria from patient samples.
Fermenting bacteria
L. iners is part of a group of fermenting bacteria that produce lactic acid as a metabolic end product. In this study, the researchers found that cancer-derived L. iners within tumors generate L-lactate, which cancer cells use instead of glucose to fuel metabolic cycles and to combat oxidative stress that occurs after radiation.
Tumor lactate and lactate dehydrogenase (LDH) expression are already associated with aggressive tumor growth and poor survival across many cancer types.
The researchers, co-led by Ann Klopp, M.D., Ph.D., professor of Radiation Oncology, were able to induce treatment resistance by introducing lactate-producing L. iners to cancer cells in vitro, resulting in the rewiring of the tumor cell metabolism to use that increased lactate.
Functions inside tumors
The results also revealed that L. iners have functions inside tumors that are not present in healthy patients, suggesting that some changes in these bacteria themselves may occur prior to cancer development.
While this study focused on L. iners, the researchers observed a strong association between other tumor-associated lactic acid-producing bacteria and poor survival across multiple cancers, noting that 40% of species are associated with RFS in subsets of lung, colorectal, skin and head and neck cancers.
Colbert and colleagues currently are developing novel approaches to specifically target these bacteria inside tumors, including topical applications to deliver anti-cancer drugs and improve patient outcomes for various cancer types.






No comments yet