A trial of a new drug regimen to treat tuberculous meningitis (TBM) has started enrolling adults and adolescents in several countries where tuberculosis (TB) is prevalent.

The Improved Management with Antimicrobial Agents Isoniazid Rifampicin Linezolid for TBM (IMAGINE-TBM) trial will compare a six-month regimen of four drugs with the nine-month, standard-of-care regimen for TBM. The study aims to generate evidence that could improve treatment for people with TBM.
IMAGINE-TBM is sponsored by the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health, and implemented through the NIAID-funded Advancing Clinical Therapeutics Globally for HIV/AIDS and Other Infections (ACTG).
Permanent disabilities
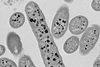
TBM is fatal in about 25-50% of adults who develop the disease and often results in permanent disabilities in survivors. It is caused by the Mycobacterium tuberculosis bacterium, which more commonly attacks the lungs and causes pulmonary TB.
In TBM, the bacteria infect the membranes surrounding the brain and spinal cord called the meninges, causing inflammation known as meningitis. This can lead to increased pressure in the brain and stroke, which often leads to neurological disability or death.
It is estimated that about a quarter of the world’s population is living with latent TB—during which M. tuberculosis bacteria remain alive in the body, but inactive—and 10% of people with latent TB become ill from the infection. Among people who develop clinical disease, up to 5% develop TBM. People living with HIV have a higher risk of death from TBM, with fatalities exceeding 50%. Although TBM is a serious illness with a high fatality rate, less is known about the optimal treatment of this disease compared with pulmonary TB.
Alternative regimens
Participants in the IMAGINE-TBM trial will be given either the investigational six-month regimen or a nine-month standard regimen. The six-month regimen will consist of high doses of rifampicin (35 mg/kg for 24 weeks) and isoniazid (15 mg/kg for the first two weeks, followed by 10 mg/kg for 22 weeks), in addition to linezolid (1200 mg) and pyrazinamide (25 mg/kg) for the first eight weeks of the treatment period.
This regimen will be compared with the current standard of care, which consists of rifampicin (10-15 mg/kg, up to 900 mg/day), isoniazid (5 mg/kg), ethambutol (20 mg/kg), and pyrazinamide (25 mg/kg) for eight weeks, followed by rifampicin (10-15 mg/kg, up to 900 mg/day) and isoniazid (5 mg/kg) for the remainder of the treatment period. Over the course of the 48-week study period, the outcomes of the trial participants will be measured by assessing their clinical status, including their neurologic and functional abilities.
The trial will include 330 participants aged 15 years and older who have or are likely to have TBM based on signs and symptoms, including people living with and without HIV. Because pregnant women are eligible to enroll in this study with appropriate consent, a small number of pregnant women are expected to be included.
Treatment options
Treatment options for adolescent children and pregnant women—groups at high risk of poor outcomes from TBM—are limited due to minimal data on the use of high-dose rifampicin and linezolid in these groups. Data from this trial could help expand treatment options for people in these groups.
Additionally, reaching patients who develop this rare form of TB can be difficult, and the disease can be hard to diagnose. The ACTG is well-positioned to conduct this study due to its strong clinical research infrastructure in countries with high rates of TB and HIV.
The study will shed light on a potentially shorter, better treatment for TBM and could result in improved outcomes for patients with this dangerous disease, saving lives and reducing neurological disabilities.






No comments yet