Fecal microbe transplants from healthy donors can treat patients with recurrent Clostridium difficile infections. However, after tens of thousands of transplants, little was known about which donor strains provide long-term engraftment, and which engraft early after the transplant. Most failures of fecal microbe transplantation occur in the first four weeks.

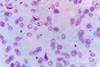
Recurrent C. difficile infections occur after suppressive antibiotic treatments that knock out almost all of the normal gut flora. Patients suffer watery diarrhea, painful abdominal cramps, a feeling of sickness, fevers and weight loss.
In 2021, researchers at the Icahn School of Medicine at Mount Sinai, New York, gave precise quantification of 150 bacterial strains belonging to 42 bacterial species that showed frequent engraftment after fecal microbial transplants. Importantly, they also tested for engraftment soon after transplant — 36 hours to four weeks — as well as later after transplantation, eight weeks to five years.
Step further
Now microbiome experts at the University of Alabama at Birmingham have taken that 2021 study, and a similar study for children who had C. difficile infections, a step further.
UAB researchers Hyunmin Koo, Ph.D., and Casey D. Morrow, Ph.D., focused on the commensal microbe Bacteroides vulgatus, one of the most common species found in healthy guts. Using DNA sequences from the two studies and powerful bioinformatics analysis, Koo and Morrow searched for genes, out of a total of 4,911 protein-encoding genes in the B. vulgatus strains, that were unique to the three B. vulgatus donors in the two studies that showed early colonization, as opposed to seven other B. vulgatus strains in the studies that did not show early colonization.
“Analysis of the common genes between the three donors revealed that only 19 were in common out of 4,911 genes encoding known and hypothetical proteins,” Morrow and Koo write in the Scientific Reports study. “The result from our analysis supports the screening of donor B. vulgatus for this gene consortium to enhance colonization following a fecal microbe transplant.”
Genes of interest
Morrow and Koo identified two of the 19 genes.
One is a putative chitobiase that the UAB researchers found was located next to genes encoding SusD, SusC, putative anti-sigma factor and RNA polymerase ECF-type sigma factor. Others previously have identified these genes as components of a commensal colonization factor complex in Bacteroides fragilis and B. vulgatus. This complex promotes a specific interaction with the host that facilitates stable, resilient colonization in mice.
“Our results, then, provide support that the commensal colonization factor complex might also function in humans to enhance the colonization of B. vulgatus,” Morrow said.
Fimbrillin family protein
The other identified gene encodes a unique fimbrillin family protein. Fimbrillins are protein polymers, previously identified in Bacteroides, that can form the hair-like structures that protrude from the surfaces of microbes and serve as anchors for microbial adhesion with host cells.
“Based on their known functions, the identification of both the chitobiase — and subsequently a complete commensal colonization factor complex — and fimbrillin proteins supports the involvement of these proteins in B. vulgatus colonization,” Morrow said.
The other 17 genes are hypothetical proteins with no identified function as yet. Interestingly, genes that mapped near the hypothetical proteins involved activities in DNA mobilization and transposition, meaning the ability to move genes into, around or out of the bacterial genome.
Weakness IDed
Morrow and Koo acknowledge a weakness in their study.
When they analyzed the 42-paired fecal microbe samples from the Human Microbiome Project data set, they found that none had the complete set of the 19 genes that were found in the three early engraftment B. vulgatus strains. Twenty-six of the samples had both the putative chitobiase and the fimbrillin genes, and another 11 had only the fimbrillin gene. There was a varied presence of the other 17 hypothetical genes in the 42 samples.
“Since none of the Human Microbiome Project pairs had the full 19 genes, we do not know whether any of the pairs would have an early colonizing phenotype in fecal microbe transplants,” Morrow said.
“Based on our analysis, we would assume that the commensal colonization factor complex and fimbrillin genes would suffice; but to resolve this issue, additional fecal microbe transplants for recurrent C. difficile in humans using early analysis times post-transplant would need to be done.”
Screening after chemo or transplant
The UAB researchers say a further application of their study could be screening following chemotherapy or transplants, which are known to involve medications that can disrupt normal microbial gut flora. “The capacity to rapidly restore the B. vulgatus community in these patients would be important to reduce the risk of infection by pathogens or antibiotic-resistant microbe pathogens that could impact overall health,” Morrow said.
Support for the Scientific Reports study, “Identification of donor Bacteroides vulgatus genes encoding proteins that correlate with early colonization following fecal transplant of patients with recurrent Clostridium difficile,” came from the Marnix E. Heersink School of Medicine at UAB. Morrow is a professor emeritus in the UAB Department of Cell, Developmental and Integrative Biology, and Koo is a bioinformatician in the UAB Department of Genetics.






No comments yet