The smell of freshly mown grass. The sweet aroma of roses. The tang of a rubbish bin on a hot summer’s day. Scents are part of the backdrop of everyday life – but research is hoping they could be used to detect diseases.
The smell of sickness
It might sound strange, but our sense of smell is actually an important evolutionary defence mechanism. Our olfactory system can seem quite humble in comparison with the more flashy senses like sight and sound, but our ability to smell is crucial. Without it, we wouldn’t be able to sniff out dangers like fires, rotten food, and even disease. If you were asked to conjure up an image of a sick person, you might think of pus, vomit, faeces, and other foul bodily secretions. I think most of us would agree that these things smell pretty bad – and there’s a reason for that. These substances can be full of harmful pathogens, as this is how they spread. By finding the scent of things like this repulsive, we are pre-programmed to avoid people who are obviously sick, thereby avoiding exposing ourselves to their harmful pathogens.

There is evidence for even more subtle chemosensory signals programmed into our brains to help us keep ourselves healthy. In 2014, a group of researchers hypothesised that it would be beneficial for humans to be able to smell sickness at the early stages of infection, before symptoms have even appeared. To test this, a group of people were exposed to lipopolysaccharide, a substance that stimulates the innate immune system to mimic the initial stages of infection. A control group were exposed to saline water only. Samples of body odour were taken before and after this treatment, and participants were asked to rate these smells based on factors like “pleasantness” and “intensity”. Fascinatingly, in people who were exposed to lipopolysaccharide, their body odour changed, being described as less pleasant. This change occurred within a few hours, and perhaps indicates an innate behavioural response to the smell of sickness, designed to protect healthy individuals. In other words, our noses tell us when something seems a bit off about someone’s health, so we avoid them like the plague.
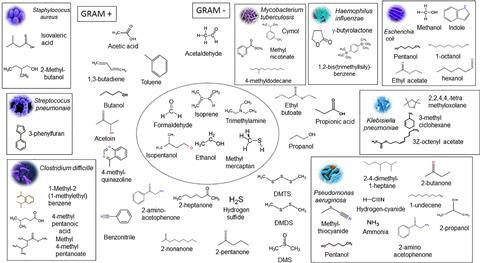
Smelly chemicals called volatile organic compounds (VOCs) are the root cause of this veritable bouquet. We produce VOCs all the time as part of our normal metabolism, but infection can change the way our body works, meaning a different assortment of VOCs are produced – resulting in a change in smell. The many microbes found on and inside our bodies also produce a lot of smells – mostly ones we’d rather not get too close to – and these can also contribute to the scent of disease.
Animal super sniffers
Many diseases are known to have a distinct smell. Some well-known examples include the sweet, fruity aroma in the breath of people with diabetic ketosis, or the meaty tang associated with Yellow Fever. Infected cutaneous wounds often have a typical “rotting” smell, while people with smallpox smell sweetish and pungent. Before modern medicine, doctors knew about the scent of disease, and used to smell or even taste bodily fluids to diagnose their patients. Much to the relief of healthcare workers worldwide, this unpleasant task has now been delegated to animals with advanced olfactory abilities.
Thanks to an abundance of anecdotal evidence, most people are familiar with dogs that can sniff out diseases. Based on this, many researchers are working on using animal noses to search for VOC biomarkers. Dogs can be trained to detect Clostridium difficile, a common cause of diarrhoea, in human stool samples, as well as urinary tract infections caused by a variety of common culprits such as Escherichia coli, Klebsiella pneumonia, Staphylococcus aureus, and Enterococcus faecalis.
Dogs aren’t the only animals being trained to smell disease. African giant pouched rats, Cricetomys gambianus, have been trained to detect tuberculosis (TB) based on the smell of sputum – the phlegmy substance produced when patients cough. Mycobacterium tuberculosis, the bacteria that causes TB, produces a characteristic aroma which the rats are trained to recognise. These rat studies have mainly been conducted by APOPO, a non-profit organisation that also trains the rats to smell land mines.

Scent-based devices
There’s no doubt that these studies are fascinating, but there are a few drawbacks to using animals in this way. First and foremost, animals take up a lot of time and money. Each critter needs adequate housing, food, and care, not to mention consistent and long-term training. No animal is correct 100% of the time, and we often still don’t know exactly what they are smelling. So, as much as I’d love to see a dog in the doctor’s office, a better long-term strategy would be to find out exactly what these animals can smell, and replicate their amazing noses using technology.
The first step in developing any kind of artificial nose is to make a list, or library, of all the VOCs associated with whatever microbe or disease you want to detect. This has to be extremely thorough – animals like dogs and rats have very sensitive noses, and can sniff out compounds that are only present in very small amounts. Mass spectrometry is normally used for this, particularly when coupled to gas chromatography. Using this analytical approach, you can find out exactly what compounds make up your sample of interest.
Next up is the nose itself. Electronic noses, or e-noses, are technological replicas of biological olfactory systems. They detect VOCs and can be programmed to recognise chemical patterns associated with specific pathogens and diseases and are already used to test for things like food spoilage – which is definitely better than subjecting human workers to a potential nose-ful of rotten food.
Nosing into the future
Early research hopes to use e-noses at the forefront of disease detection, particularly when the only alternatives are expensive, invasive, or painful for the patient. Many diseases have non-specific symptoms, particularly at the early stages, with patients just seeming generally ‘unwell’. A great example of this is TB; early signs of this infection include weight loss, difficulty sleeping, and a phlegmy cough, which could easily be the signs of several other diseases. Instead of putting patients through a series of time-consuming diagnostic tests to find out what exactly is wrong with them, it would be fantastic if an e-nose or other smell-based test could do the difficult part for us.
Of course, things aren’t that simple. Finding smelly biomarkers that actually work reliably is much easier said than done, and the infected body produces so many VOCs that it can be challenging to untangle the whole picture and narrow it down to just the chemicals that count. Factors like age, gender, body mass index, and ethnicity can change the VOCs a person produces, and even your diet can alter the way you smell – the unpleasant aftermath of eating garlic or asparagus is just the beginning. Advances in ‘omics’ methods, such as metabolomics and proteomics, are helping, as are the constant developments in machine learning and data processing, but there is still a long way to go.
Smell-based disease diagnosis is an exciting field of research, but while we are getting closer to reliably sniffing out sickness in the clinic, we still have a lot of work to do. But who knows – the next big breakthrough could be right under our noses.

Read more: Bridging the gap: mouse breath research to advance infectious disease diagnostics










No comments yet