New HIV transmissions in England have fallen by almost a third since 2019, while fewer people remain unaware of their HIV status as a result of increased testing across the country, according to an update on the HIV Action Plan for England.
As part of the HIV Action Plan, NHS England is investing £20 million in the 3 years from 2022 to 2023 to 2024 to 2025 to expand blood borne viruses opt out testing in emergency departments in the local authority areas across the country with the highest prevalence of HIV: London, Brighton, Manchester, Salford and Blackpool.
The new report published shows this expanded testing has helped diagnose 2,000 cases of blood-borne viruses - including 343 people living with HIV - in the first year of the programme.
HIV prevention
Another major commitment was the investment of over £3.5 million to deliver a national HIV prevention programme between 2021 to 2024 to raise awareness of HIV and sexually transmitted infections testing and prevention strategies.
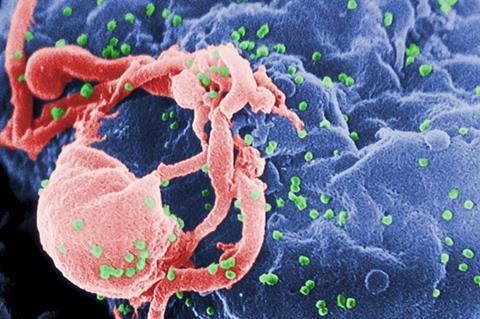
Reducing undiagnosed HIV infection through testing not only provides access to treatment that saves lives but means people who obtain undetectable levels of the virus cannot pass on HIV. During National HIV Testing Week 2023 almost 22,000 HIV testing kits were ordered - with self-testing kits (providing instant at-home results) available for the first time.
Progress made
Health Minister Neil O’Brien said: ”It’s hugely encouraging to see the progress made so far in our goal to end new HIV transmissions as well as AIDS and HIV-related deaths in England by 2030.
“Since the HIV Action Plan was launched in 2019, we have been working hard to reduce new infections by tackling stigma and urging more people to get tested, as well as helping people to access potentially life-saving treatment.
“Regardless of sexual orientation - people should get tested regularly for HIV, so we can drive down infections further.”
Late HIV diagnoses
Professor Kevin Fenton, government’s Chief Advisor on HIV and Chair of HIV Action Plan Implementation Steering Group said: ”It’s positive to see new HIV diagnoses continue to fall, but our work is not done - late HIV diagnoses remain high in England which sadly increases the risk of death.
“Improving quality of life for people living with HIV and addressing stigma is a key objective in our HIV Action Plan and we will continue working with UKHSA and key delivery partners to understand, measure and address stigma in all its forms.
“We are very thankful to our many partners from government, NHS, local government and communities across the country who are working together to drive progress on the action plan. It is only through collective, focused action on ending HIV transmissions that we will be successful.”
PrEP treatment
Pre-exposure prophylaxis treatment (PrEP) is available to individuals with negative HIV status but that could be at higher risk of HIV infection - for example, those whose partner is HIV positive.
To improve PrEP uptake, the PrEP Access and Equity Task and Finish Group - set up in September 2022 and chaired by the Association of Directors of Public Health and Terrence Higgins Trust - has gathered evidence to help break down barriers to eligible people accessing the treatment. Recommendations were presented to the HIV Action Plan Implementation Steering Group and will inform the development of a roadmap to improve PrEP access and equity.
Undiagnosed HIV
According to the HIV Action Plan monitoring and evaluation framework published by the UK Health Security Agency (UKHSA) in December 2022, the estimated number of people living with undiagnosed HIV in England fell by more than one thousand from 2019 to 2021, from 5,600 to 4,400.
The number of people attending sexual health services due to their partner receiving a notification of positive HIV diagnosis also fell by almost half for the same time period, from 1,558 to 820.
Prof Susan Hopkins, Chief Medical Advisor at the UK Health Security Agency, said: ”The end of HIV transmission is in sight in England, but increasing testing, access to prevention including PrEP and getting those diagnosed started on HIV treatment earlier is crucial to achieving this goal. Taking treatment if you are living with HIV so that the virus is undetectable prevents transmission.
“No matter your gender or sexual orientation, getting regularly tested, using condoms and PrEP (if you’re eligible), are essential to protect your and your partners health.”
Steering group
To drive progress, a national HIV Action Plan Implementation Steering Group (HIVAP ISG) has been created and is chaired by Professor Kevin Fenton, who has also been appointed the government’s Chief Advisor on HIV. The national HIV Action Plan Implementation Steering Group includes all key partners, including the voluntary sector.
DHSC has also created a Community Advisory Group, chaired by the National AIDS Trust and the LGBT Foundation, to advise the HIV Action Plan Implementation Steering Group through the lifetime of the HIV Action Plan.
Many areas of the country have replicated this national action regionally, providing leadership and oversight of work underway within local systems. This has seen regional HIV action plans developed in areas such as the South West, working groups set up in the Midlands, stocktakes of testing activity and action via Sexual Health Networks in the South East and North East and Yorkshire, or regional HIV Action Planning Workshops as in the East of England.







No comments yet