The University of Oxford has launched a new clinical trial to test a vaccine to protect people against deadly Nipah virus.
This is the first-in-human trial of the ChAdOx1 NipahB vaccine, being developed by researchers at the University of Oxford’s Pandemic Sciences Institute. Fifty-one people aged 18 to 55 will participate in the trial, which will be led by the Oxford Vaccine Group and is funded by the Coalition for Epidemic Preparedness Innovations (CEPI).
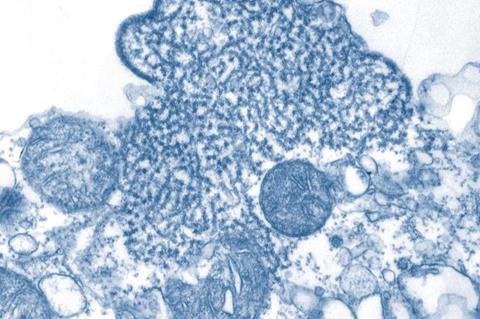
Nipah virus is a devastating disease that can be fatal in around 75% of cases. Outbreaks have occurred in countries in South-East Asia, including Singapore, Malaysia, Bangladesh and India, with a recent outbreak in Kerala, India in September 2023. Nipah virus is carried by fruit bats and may also be transmitted by contact with infected animals (such as pigs) or from person-to-person via close contact.
Priority disease
The virus, which is recognised by the World Health Organization as a priority disease requiring urgent research, belongs to the same family of paramyxoviruses as more well-known pathogens like measles. Despite the first outbreaks of Nipah virus occurring 25 years ago in Malaysia and Singapore, there are currently no approved vaccines or treatments.
Professor Brian Angus, the trial’s Principal Investigator and Professor and Reader in Infectious Diseases at the Centre for Clinical Tropical Medicine and Global Health in the University of Oxford’s Nuffield Department of Medicine said: “Nipah virus was first identified in 1998, and yet 25 years on the global health community still has no approved vaccines or treatments for this devastating disease.
“Due to the high mortality rate and the nature of Nipah virus transmission, the disease is identified as a priority pandemic pathogen. This vaccine trial is an important milestone in identifying a solution that could prevent local outbreaks occurring, while also helping the world prepare for a future global pandemic.”
Epidemic potential
Dr In-Kyu Yoon, Acting Executive Director of Vaccine Research & Development at CEPI, funders of the trial and one of the leading global funders of Nipah virus research, said: “Nipah has epidemic potential, with its fruit bat hosts found in areas home to over two billion people. This trial is a step forward in efforts to build a suite of tools to protect against this killer virus. Knowledge gained could also inform development of other Paramyxovirus countermeasures.”
The University of Oxford has produced the vaccine against Nipah virus using the ChAdOx1 platform, the same viral vector vaccine platform that was used for the Oxford/AstraZeneca COVID-19 vaccine, and that has saved an estimated 6 million lives worldwide.
The project will run over the next 18 months, with further trials expected to follow in a Nipah-affected country.
The vaccine trial is a key part of the Pandemic Sciences Institute’s Henipavirus Programme, which is working with partners in endemic countries to develop practical tools that will ensure the world is better prepared for future outbreaks. This includes providing world-leading biomedical research and developing ethical frameworks to minimise stigma from the disease.
Nipah disease factfile
- Nipah virus belongs to the same family of paramyxoviruses as more well-known pathogens such as measles.
- Nipah virus is carried by fruit bats and infects people when they eat food that is contaminated with bat urine or saliva containing the virus. It may also be transmitted by contact with infected animals (such as pigs) or from person-to-person via close contact.
- Although symptoms of Nipah virus infection can be mild, more severe cases result in devastating disease involving the central nervous system (encephalitis, coma), respiratory system, or death. Severe disease is fatal in up to 75% of cases and survivors can be left with long-term neurological complications.
- There are currently no approved vaccines or treatments for Nipah virus infection.
- Nipah virus is a World Health Organization and UK Vaccine Network priority pathogen based on the severity of the illness, the high risk of mortality, the possibility of person to person spread, and the lack of vaccines and treatments.
- To date, Nipah outbreaks have occurred in countries in South-East Asia, including Singapore, Malaysia, Bangladesh and India. Seasonal outbreaks have occurred annually in Bangladesh since 2001. India has seen four outbreaks including a recent outbreak in Kerala in September 2023, with a virus that is related to but distinct from the strain circulating in Bangladesh.







No comments yet