Among the more than 100 types of human papillomavirus (HPV), at least 14 are considered as ‘high-risk’ types which can cause (cervical) cancer. After breast cancer, cervical cancer is the most common cancer in Europe among women aged 15–44 years [1].

Before HPV vaccination among teenage girls started in Denmark, high-risk HPV was found in all cervical cancers. HPV types 16/18 accounted for around three quarters (74%) of cervical cancers. These two types are covered in the 4-valent HPV vaccine offered to girls since 2008 as well as the 9-valent vaccine which has been in use in Denmark since November 2017. One third (26%) of cervical cancers prior to the HPV immunisation campaign were caused by high-risk types that are not covered by the 2- and 4-valent vaccine.
READ MORE: Growing body of evidence links HPV with heart disease
READ MORE: Comprehensive meta-analysis pinpoints what vaccination strategies different countries should adopt
In their research article published in Eurosurveillance, Nonboe et al. examined the HPV status of cervical samples over time among women (22–30 years) at screening age for cervical cancer who were vaccinated as girls [2].
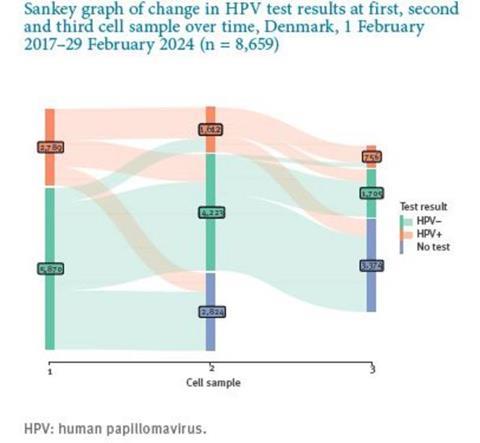
They tested up to three consecutive cervical cell samples per participant provided by the contributing pathology departments in Denmark for HPV. In total, 17,252 women with at least one cervical cell sample were registered between 1 February 2017 and 29 February 2024. During the seven years of the randomised “Trial23” study (cervical cancer screening starts at age 23 in Denmark), 84% of women in the study had at least one cell sample taken. The authors compared HPV prevalence, persistence and incidence among vaccinated and unvaccinated women.
Strong indication
Based on the data gathered during the study period, HPV16/18 has been almost eliminated among vaccinated women in Denmark: prevalence of these two types in the samples decreased to < 1% in 2021 from 15–17% before vaccination of girls. In addition, prevalence of the types 16/18 in women who had not been vaccinated against HPV remained at 5% which, according to the authors, “strongly indicates population immunity”.
Despite the evidence of protection through vaccination, about one third of women screened during the study period still had HPV infection with high-risk HPV types not covered by the offered vaccines — and new infections with these types were more frequent in vaccinated than in unvaccinated women.
There was a low prevalence of HPV16/18 during the 7-year study period and women who have been vaccinated against HPV as girls are expected to have a considerably lower risk of cervical cancer compared with previous generations. Therefore, the authors also assessed whether the current cervical screening strategies in the country could be adjusted accordingly or even stopped entirely.
Screening age
The study results showed a remaining high prevalence of high-risk HPV infections in women that are not covered by the HPV vaccines and that had been detected both in vaccinated and unvaccinated women during the study period. At the same time, the authors noted a significantly higher incidence of non-vaccine high-risk HPV types among vaccinated women than in unvaccinated women.
Based on this, Nonboe et al. thus conclude that “less intensive screening seems reasonable until women vaccinated as girls with the 9-valent vaccine reach screening age, at which point screening should be reconsidered.”
[1] Read more on the European Vaccination Information Portal: https://vaccination-info.europa.eu/en/human-papillomavirus-hpv
[2] Nonboe Mette Hartmann, Napolitano George Maria, Schroll Jeppe Bennekou, Andersen Berit, Bennetsen Mary Holten, Christiansen Sanne, Frandsen Anna Poulsgaard, Rygaard Carsten, Salmani Rouzbeh, Høgdall Estrid Vilma Solyom, Lynge Elsebeth. Human papillomavirus prevalence in first, second and third cervical cell samples from women HPV-vaccinated as girls, Denmark, 2017 to 2024: data from the Trial23 cohort study. Euro Surveill. 2025;30(27):pii=2400820. https://www.eurosurveillance.org/content/10.2807/1560-7917.ES.2025.30.27.2400820
[3] Three prophylactic HPV-vaccines are licensed by the European Medical Agency (EMA) for use in European countries. The 4-valent HPV vaccine covers high-risk HPV types 16/18 and low-risk types 6/11. The 2-valent covers HPV types 16/18 and the 9-valent vaccine covers HPV types 6/11/16/18/31/33/45/52/58. The high-risk HPV types covered by the 2-valent and 4-valent are responsible for 70% of cervical cancers, and the high-risk HPV types covered by the 9-valent vaccine are responsible for up to 90% of cervical cancers.






No comments yet