Prof. Gabriel Nussbaum and his team at the Institute of Biomedical and Oral Research, Hebrew University-Hadassah Faculty of Dental Medicine, have recently published groundbreaking research in the journal Gut, uncovering a pivotal link between oral bacteria and the onset of pancreatic cancer in mice.
Their study delves into the intricate relationship between oral microbiota, notably Porphyromonas gingivalis, and the acceleration of pancreatic cancer development, offering crucial insights into early detection, prevention, and potential therapeutic avenues.
Pancreatic ductal adenocarcinoma (PDAC) has been connected to the presence of Porphyromonas gingivalis, a prevalent anaerobic bacterium known for its association with periodontal disease. Leveraging epidemiological clues, Prof. Nussbaum’s team embarked on a journey to elucidate the potential of P. gingivalis in driving the progression of pancreatic cancer.
Accelerated cancer development
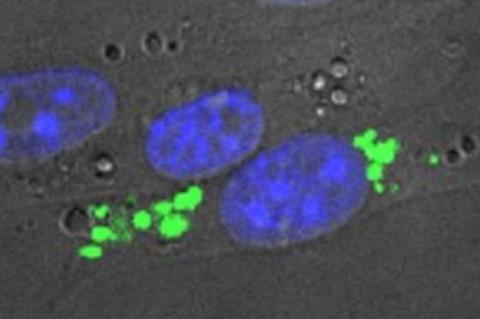
Their research entailed a comprehensive examination of P. gingivalis translocation from the oral cavity to the pancreas using mouse models. By introducing the bacterium to genetically engineered mice predisposed to PDAC, the team uncovered compelling evidence of accelerated cancer development.
Key findings from the study indicate that viable P. gingivalis was found in the pancreas of healthy mice after applying it to the gums, and prolonged exposure caused changes in the pancreas, affecting its microbial balance. Additionally, applying P. gingivalis orally sped up the progression from early pancreatic abnormalities to pancreatic cancer in mice with a specific genetic mutation.
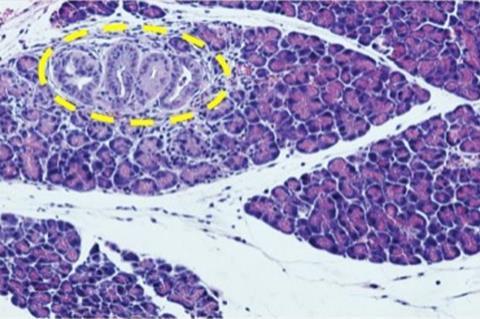
The research also showed that this genetic mutation helped P. gingivalis survive inside cells, and the bacteria supported the survival of pancreatic cancer cells even when conditions were tough. Prof. Nussbaum and his team’s discoveries emphasize a direct link between P. gingivalis and the development of pancreatic cancer in mice, offering significant insights into how this disease progresses.
Oral health
“The study underscores the significance of considering oral health in understanding and tackling pancreatic cancer,” says Prof. Gabriel Nussbaum, lead researcher at the Institute of Biomedical and Oral Research. “By exploring the role of bacteria like P. gingivalis, we’re not only shedding light on potential risk factors but also uncovering new avenues for intervention and treatment.”
The findings suggest that there’s a real possibility that gum disease could be connected to the risk of pancreatic cancer, emphasizing how bacteria directly affect this link. There’s potential in focusing on bacteria within cells as a way to lower the risk of pancreatic cancer or to improve existing treatments for it. These insights open up avenues for future research and could lead to more effective strategies for preventing and treating pancreatic cancer.







No comments yet