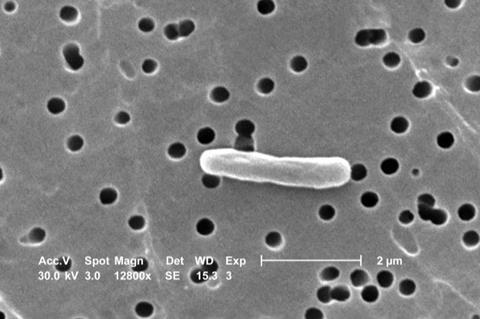
A milestone study led by University of Queensland researchers has identified the main types of E. coli bacteria that cause neonatal meningitis, and revealed why some infections recur despite being treated with antibiotics.
Professor Mark Schembri and Dr Nhu Nguyen from UQ’s Institute for Molecular Bioscience and Associate Professor Adam Irwin from UQ’s Centre for Clinical Research led a team which discovered that around 50 per cent of neonatal meningitis infections are caused by two types of E. coli.
“Neonatal meningitis is a rare but life-threatening disease that occurs when a newborn baby is infected with bacteria,” Professor Schembri said.
“E. coli is the most common cause of meningitis in babies born pre-term, but knowing which types allows us to test for those strains and treat them appropriately.”
Largest ever study
The study was the largest ever of its type, examining the genomes of 58 different E. coli bacteria across four continents and using samples collected over 46 years.
It found two types of the bacteria were responsible for the majority of neonatal infections.
Associate Professor Irwin, who is also a paediatric infectious disease specialist at the Queensland Children’s Hospital, said meningitis can have a devastating impact on families.
“Parents may lose their child, or in a significant proportion of cases the child can suffer ongoing complications such as a brain injury, leading to developmental problems,” Dr Irwin said.
“While antibiotics can be effective in treating the infection, this relies on rapid diagnosis.
Repeat offenders
“Also, antibiotics don’t always eliminate the bacteria – some of the babies we tracked showed signs of a complete recovery before suffering repeated invasive E. coli infections.”
The researchers discovered the bacteria causing subsequent infections were the same as in the initial infection.
“It’s most likely that bacteria hide out in the intestinal microbiome,” Professoe Schembri said.
“This tells us we need to keep monitoring these babies after their first infection, as they are at a high risk of subsequent infection.”
Double action
Professor Schembri said the E. coli that can lead to meningitis also cause urinary tract infections and colonise the intestinal tract.
“There is something about these types of E. coli that equips them to cause both infections,” he said.
“Our next step is to examine the bacteria’s pathway from the intestinal tract or urinary tract into the bloodstream, and then to the brain, so we can consider new ways to stop them.”
Professor Schembri is a co-affiliate of UQ’s School of Chemistry & Molecular Biosciences.
Australian collaborators on the research included Dr Brian Forde (UQ’s Institute for Molecular Bioscience), Dr Patrick Harris (UQ Centre for Clinical Research), Associate Professor Scott Beatson (School of Chemistry and Molecular Biosciences), Dr Sanmarie Schlebusch (UQ Centre for Clinical Research) and Dr Haakon Bergh (Pathology Queensland).
The research was funded by the Children’s Hospital Foundation, the National Health and Medical Research Foundation, the Wellcome Trust and The University of Queensland.
The research paper was published in eLife.
Video: https://youtu.be/CfbwHPc_6OM







No comments yet