Antimicrobial resistance – occurring when pathogens can survive antibiotic treatment – is one of the most rapidly emerging global public health threats today. According to a 2022 study, nearly five million deaths were associated with antibiotic-resistant bacteria in 2019, with over a million deaths per year directly attributable to antimicrobial resistance.
In a new study, researchers from the Typas Group at EMBL Heidelberg have systematically profiled over 10,000 drug combinations for their effectiveness against common multidrug-resistant bacteria.
“Previously, there have been studies on specific drug combinations, especially those commonly prescribed together in the clinic,” said Elisabetta Cacace, the first author of the study and former PhD student in the Typas group. “However, we lacked systematic knowledge of how combinations of different classes of antibiotics, or combinations of antibiotics and non-antibiotic drugs, influence bacterial physiology, especially when considered independently of the host.”
Antibiotics in combination
Cacace, who is trained as a medical doctor and is currently a postdoc at ETH Zürich, has been interested in antimicrobial resistance since early in her career. During her time in the Typas Group, which specialises in developing high-throughput approaches to studying bacterial interactions (with the environment or other species) and physiology, she turned her attention to the problem of understanding how antibiotics influence each other’s actions on their cellular targets.
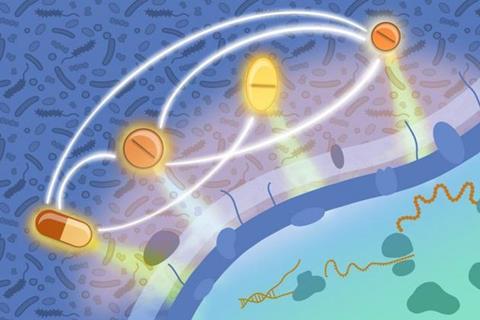
Different antibiotics target different cellular structures or processes inside bacteria. They can synergise, which means their combined activity is more potent than the effect of each drug alone, but they can also antagonise each other, in which case the presence of one drug hampers the activity of another. Such antagonising interactions can be used to mitigate the collateral damage of antibiotics on our gut microbiota.
In a previous study, researchers from the Typas Group had profiled drug combinations against Gram-negative bacteria – a class that includes many deadly antimicrobial-resistant pathogens, including E. coli, Salmonella enterica, and Pseudomonas aeruginosa.
However, many deadly antimicrobial-resistant bacteria also belong to the Gram-positive category, including Staphylococcus aureus, whose methicillin-resistant variant (MRSA) causes hundreds of thousands of deaths each year. These bacteria have a different cell wall structure to Gram-negative bacteria, which influences the activity and effectiveness of drugs.
Robotics set-up
For the current study, the team used a sophisticated robotics set-up to simultaneously study the effects of hundreds of combinations of antibiotic and non-antibiotic drugs, across a range of doses, on three representative species of Gram-positive bacteria – Bacillus subtilis, Staphylococcus aureus, and Streptococcus pneumoniae.
In addition to more than 8,000 combinations of 65 different antibiotics, spread across all major classes, the researchers also profiled over 2,500 combinations of antibiotic drugs with non-antibiotic drugs, which may be co-prescribed in an age where polypharmacy – simultaneous use of multiple medications – is very common.
Using this strategy, the team identified more than a thousand interactions, including both synergies and antagonisms. The effects were highly species- and even strain-specific, and distinct from the interactions seen in the previous study in Gram-negative bacteria. They also validated some of these results in vivo, by infecting moth larvae with the pathogen and testing the ability of specific drug combinations to aid in recovery.
Open access database
The researchers have made the full database of interactions openly available for other scientists to view, explore, and use to search for new synergies and antagonisms.
“We think the scale of this study really sets it apart. This is such a rich dataset that I think it will feed hypotheses for many years to come,” said Cacace. “I also find it interesting from a systems biology perspective, because we see interactions between drugs targeting certain cellular processes that were not known before.”
“We are living in an era when novel strategies against antimicrobial resistance are desperately needed, and the development of new antibiotics is technically challenging, costly, and time-consuming,” said Nassos Typas, EMBL Group Leader and the study’s senior author. “Systematic drug interaction profiling of the kind we have performed in this study opens up the path to alternative solutions and treatments for bacterial infections.”







No comments yet