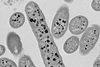
Research from the University of Kansas just published in Proceedings of the National Academy of Sciences could hasten development of a new class of vaccines aimed at SARS-CoV-2, the virus that causes COVID-19.

Anthony Fehr, associate professor of molecular biosciences, led research into a protein dubbed ‘Mac1’, which has intrigued molecular bioscientists as an antiviral target because it’s known to help confer virulence, or the power to cause disease. Results have spurred several groups, including the Fehr lab, to begin developing novel inhibitors of Mac1.
“We’ve built up a body of literature showing this gene is critical for the virus to cause disease,” Fehr said. “To better understand this protein, we use what’s called reverse genetics, where we can delete or mutate this gene so it no longer functions in the context of the actual virus. While we’ve done this in a lot of different coronaviruses, we hadn’t actually explored this in SARS-CoV-2 until just recently. This paper really describes our efforts to get rid of this protein Mac1 in SARS-CoV-2 and really see what’s happening.”
Strong target
Studying how SARS-CoV-2 behaved in mouse models, Fehr’s collaborator at Oklahoma State, Rudra Channappanavar and his group, found that without Mac1, the virus barely had an impact on the health of mice.
“If you look at the mouse data, we find that every mouse survived and showed no real signs of disease when they were infected with the virus without this gene, whereas when we give mice the normal virus — we would call it the ‘wild-type’ virus — every mouse dies,” Fehr said. “So, there’s a huge discrepancy in the ability of those viruses to cause disease. These results further demonstrate that Mac1 is a strong target for the development of novel antiviral therapies.”
What’s more, Fehr and his co-authors found the virus, without the Mac1 protein, induced a robust initial immune response in mice, the kind of biological response researchers look for in a vaccine target.
Innate immune response
“That first response you have to a virus, called an innate immune response, is dramatically increased in this infection,” said the KU researcher. “When we infect the mice, this further improves the adaptive immune response, which is that T- and B-cell response we get that produces antibodies and antiviral T-cells later on — that can really protect us from future disease.”
Fehr and Channappanavar have already shown that prior infection with the attenuated virus can be protective for mice from a future infection.
“Right now, we’re really looking at further developing this virus into a live attenuated vaccine for SARS-CoV-2, and we’re working on different strategies with minor modifications to this virus to make it even better,” he said. “We think this is a great start to developing a vaccine that we think would have longer lasting immunity.”
Intranasal vaccine
Fehr said such a vaccine could be administered intranasally, targeting the lung, giving it advantages over today’s recommended vaccine regimen based on mRNA technology.
“One of the major problems with the current vaccines is that we give them in your arm — when you give a vaccine in your arm or your muscle, you don’t really get great immune responses in your lungs,” he said. “We think that live-attenuated vaccines given intranasally can improve that response.”
Additionally, live-attenuated COVID-19 vaccines could last longer than current vaccines requiring boosters.
“I don’t want to dis mRNA vaccines — they’re great,” Fehr said. “But they’re not particularly long-lasting. We’re finding their immunity wanes over the course of time. Live-attenuated viruses have been around for decades, and many of them are very effective and last very long. We can get a lot of live-attenuated vaccines as children, and we never have to take them again because they last our lifetime.”
Unchanging regions
According to Fehr, a live-attenuated vaccine would target parts of the virus more likely to remain the same from variant to variant.
“All the current vaccines out there are really focused on a small portion of that spike glycoprotein that’s on the outside surface of the virus,” Fehr said. “There are a lot of parts of that that don’t change, and they’re sensitive to the current vaccines. But if there are changes in the spike protein, will those vaccines keep working? Mostly, they do. But some of them do lose efficacy.”
Fehr said a whole-virus vaccine, like the one his lab is investigating, could target regions of the genome that don’t change from variant to variant.
“It could reduce what I call ‘variant chasing’ that we have with a lot of our different vaccines now,” he said. “Hopefully this approach targeting the Mac1 could be beneficial in preventing disease from future variants.”
Collaboration
Fehr’s KU collaborators were lead author Yousef M. Alhammad, a former postdoctoral researcher, along with postdoctoral researcher Srivatsan Parthasarathy, doctoral students Joseph O’Connor, Catherine Kerr and Jessica Pfannenstiel; and Robert Unckless, associate professor of molecular biosciences, Edward & Thelma Wohlgemuth Faculty Scholar and director of the KU Center for Genomics. They were joined by co-authors Roshan Ghimire, Debarati Chanda, Caden Miller, Sunil More and Rudragouda Channappanavar from Oklahoma State University and Sonia Zuniga and Luis Enjuanes of the National Centre for Biotechnology, Campus Universidad Autónoma de Madrid in Spain.
“I’m really proud of this group. We all came together, worked really hard and produced some really great science,” Fehr said.
The work was funded at in part by grants from the NIH and with significant support from the Chemical Biology and Infectious Disease COBRE at KU, led by Scott Hefty, professor and chair of molecular biosciences at KU, and startup funds from KU and Oklahoma State University.
Topics
- Anthony Fehr
- Caden Miller
- Campus Universidad Autónoma de Madrid
- Catherine Kerr
- COVID-19
- Debarati Chanda
- Jessica Pfannenstiel
- Joseph O’Connor
- live-attenuated vaccines
- Luis Enjuanes
- Mac1
- Oklahoma State University
- One Health
- Research News
- Robert Unckless
- Roshan Ghimire
- Rudra Channappanavar
- SARS-CoV-2
- Sonia Zuniga
- Srivatsan Parthasarathy
- Sunil More
- University of Kansas
- USA & Canada
- Vaccinology
- Viruses
- Yousef M. Alhammad






No comments yet