The human papillomavirus, or HPV, vaccine is cutting cases of cervical cancer right across the socio-economic spectrum, with most cases being prevented in more deprived groups, according to a major study funded by Cancer Research UK.
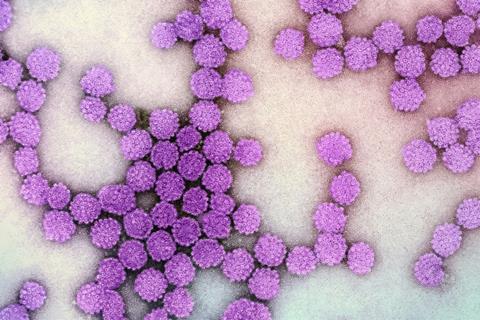
Until now, there had been concerns that the HPV vaccine could have an unequal impact across society. After carrying out the longest follow-up on the effectiveness of the HPV vaccine, researchers at Queen Mary University of London concluded the HPV vaccination programme in England is helping to close some inequalities in cervical cancer.
Due to a typically higher incidence of cervical cancer in more deprived groups, researchers found that more cases were prevented in the most deprived group (around 190), compared to the least deprived group (around 60).
Health inequalities
Published in the BMJ medical journal, the data reflected the huge success of the school-based vaccination programme, showing that well-executed public health interventions can help to reduce health inequalities.
Today’s news adds even more weight to evidence that HPV vaccination works. Researchers found that over a 12-year period, the vaccine reduced cervical cancer incidence rates by nearly 90% and pre-cancerous conditions by around 95% in women who were offered routine vaccination at 12-13 years old in England. The study shows that the vaccine is much more effective when taken up by people in year 8 (aged 12-13) than later in life.
Although the life-saving HPV vaccine currently reaches people from all backgrounds, Cancer Research UK warns that some inequalities remain in cervical cancer incidence, and more work is needed to improve the health of the most deprived groups. Uptake of the HPV vaccine in the UK has also fallen in recent years.
Overall, cervical cancer rates are higher in people from deprived backgrounds across the UK. Researchers said this is partly due to people being at greater risk from HPV and barriers that can drive lower screening attendance.
Cervical cancer
Professor Peter Sasieni, lead author from Queen Mary University of London, said: “Our research highlights the power of HPV vaccination to benefit people across all social groups.
“Historically, cervical cancer has had greater health inequalities than almost any other cancer and there was concern that HPV vaccination may not reach those at greatest risk. Instead, this study captures the huge success of the school-based vaccination programme in helping to close these gaps and reach people from even the most deprived communities.
“In the UK, the elimination of cervical cancer as a public health problem in our lifetime is possible with continued action to improve access to vaccination and screening for all.”
Public health problem
The HPV vaccine, combined with cervical screening, can dramatically reduce cervical cancer incidence to the point where almost no one develops it. Improving people’s access to both programmes is at the heart of NHS England’s recent pledge to eliminate cervical cancer as a public health problem by 2040.
This research, however, lands when uptake of the HPV vaccine and screening attendance has fallen in recent years across the UK and coverage rates are yet to recover from the disruption of the COVID pandemic.
With huge progress in tackling cervical cancer at risk of stalling, Cancer Research UK is encouraging all eligible people to take up the offer of vaccination and screening. The charity is also calling on the UK Government to ensure both programmes in England are backed by sufficient resources and modern IT infrastructure.
HPV vaccination works
Cancer Research UK’s senior health information manager, Sophia Lowes, said: “Every year, around 3,300 people receive a cervical cancer diagnosis in the UK. This research shows us that HPV vaccination works, and increased coverage can help to bring about a future virtually free from this disease.
“But we can’t lose momentum. We’re calling for targeted action to ensure that as many young people as possible get the lifesaving HPV vaccine. Better reporting on uptake by deprivation and ethnicity, along with more research, will help us understand how to reach those most at risk.
“We encourage people to take up the HPV vaccine if they are eligible. If you are concerned that you or your child has missed out on the HPV vaccine, you can contact your child’s school nurse, school immunisation service or GP surgery to find out more.”
Dropping cervical cancer rates
Cancer Research UK scientists helped to prove the link between HPV and cervical cancer 25 years ago. This discovery put the gears in motion for the HPV vaccination programme and improved cervical cancer screening. Thanks to these scientific developments, cervical cancer rates in the UK have fallen by almost a third since the early 1990s.
The HPV vaccination programme was first introduced to England in 2008. Since then, girls aged 11-13 in the UK have been offered the vaccine and since September 2019, boys of the same age can also get it. Anyone who missed their vaccine can request it through the NHS up to the age of 25.
It’s also available to men who have sex with men and some transgender people up to the age of 45 through sexual health and HIV clinics.
Promising news
Cancer Research UK chief executive, Michelle Mitchell OBE, said: “Today’s news is promising – the HPV vaccination programme is paving the way to make cervical cancer a rare disease for all.
“The UK Government and the NHS must continue to work with communities and services, so the HPV vaccine is taken up by as many eligible people as possible, and accurate information reaches those who most need it.
“We want to see a world where everyone shares in this scientific and research progress equally.”






No comments yet