A new model system for studying mpox virus infections in the laboratory is providing valuable insights into the virus’s mechanisms of attack on skin cells, offering a potential catalyst in the quest to discover innovative drugs to combat this emerging pathogen.
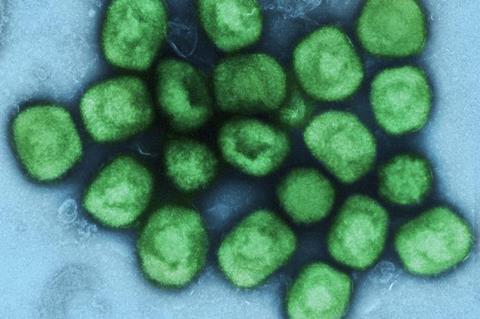
An international research team that included KAUST scientists has demonstrated that lab-grown human skin — stem cell–derived 3D structures called organoids — can effectively facilitate the active replication of mpox virus, the virus formerly known as monkeypox virus, that spread rapidly during a major outbreak in 2022.
“Researchers can now use this model to study how the mpox virus causes disease and to test new therapeutics,” says Intikhab Alam, a bioinformatician who contributed to the study along with his colleague Roberto Incitti, both from KAUST.
Lesion lessons
People infected with the mpox virus typically develop rashes and skin lesions, often leading to scarring and disfigurement — and the lab-grown skin organoids now help show why.
KAUST’s Alam and Incitti collaborated with Qiuwei Abdullah Pan and his team from the Erasmus MC-University Medical Center in Rotterdam to report that the virus takes up residence inside keratinocytes, the predominant cell type in the skin’s outer layer. There, the virus undergoes its four steps of assembly, a process that the researchers could observe under high-power microscopes.
Gene expression analyses conducted by the researchers revealed that numerous viral genes become activated in the days following infection. This activation, in turn, appears to induce changes in host cells, leading to alterations in the activity of multiple human genes associated with immunity and cell death.
These genetic alterations likely compromise the skin’s protective barrier, resulting in the characteristic lesions observed in infected people.
Reversing the effects
The observed effects could be reversed through use of an antiviral drug called tecovirimat. In the infected organoids, this drug proved highly effective in halting virus replication and thwarting the subversion of host cells.
The findings validate the mpox-inhibiting potential of tecovirimat, a drug approved to treat infections with the related smallpox virus. They also underscore the potential of the organoid system as a versatile platform with which to screen for novel substances with similar properties.
Notably, the impact of mpox extends beyond skin-related issues. In severe cases, the virus can wreak havoc on internal organs. The same KAUST-affiliated research team previously developed a kidney organoid system designed to study mpox infections in renal tissues. Other groups have investigated mpox dynamics within colon and brain organoids.
“These studies all complement each other by modeling infection in different tissues and with different types of disease manifestations,” says Incitti.
Collectively, the efforts in organoid models — which the KAUST researchers and their collaborators are now extending to other viral infection systems as well — should “help to combat the current mpox outbreak and enhance pandemic preparedness for the future,” Incitti says.







No comments yet