The University of Rochester will house a new national center focused on using tissue-on-chip technology to develop drugs more rapidly and reduce the need for animal trials.
The National Institutes of Health awarded a $7.5 million grant to establish the Translational Center for Barrier Microphysiological Systems (TraCe-bMPS) at Rochester in partnership with Duke University.
The center aims to develop five Food and Drug Administration–qualified drug development tools related to study barrier functions in disease - interfaces in tissue that are critical for the progression of infection, cancer, and many autoimmune disorders. Over the five-year grant, the researchers will create drug development tools specifically related to central nervous system disorders, fibrosis, musculoskeletal autoimmune disease, sepsis, and osteomyelitis.
Microphysiological systems
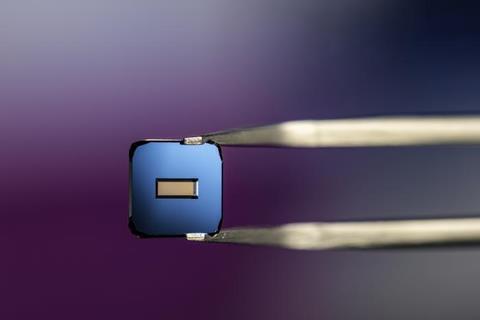
The TraCe-bMPS scientists will create the drug development tools using microphysiological systems—small chips with ultrathin membranes of human cells. They will be built using the modular, mass-producible µSiM chips pioneered by center director James McGrath, the William R. Kenan Jr. Professor of Biomedical Engineering.
McGrath says that testing drugs on µSiM chips can lead to fewer animal trials. And because researchers will be studying the drugs’ effects on human cells, they may also help overcome some of the critical differences between testing on humans and animals.
“Drug discovery is moving into an era where fewer animals are used to test for safety and efficacy,” says McGrath. “Instead, more screening will be done on tissue chips that pattern human cells in a way that mimics human tissue and disease. Our chips are designed to provide the higher throughput and more reliable indications that pharmaceutical companies need to get their drugs approved for clinical trials and use by patients.”
Elegant fusion
Hani Awad, the Donald and Mary Clark Distinguished Professor in Orthopaedics and a professor of biomedical engineering, will serve as the associate director for development. He says Congress passing the FDA Modernization Act 2.0 in 2022 made the center possible and that the team is excited to help shape the future of drug development.
“The timing could not be more perfect,” says Awad. “As a biomedical engineer and scientist, I find the elegant fusion of engineering and biology inherent in the design and validation of these tissue chips as disease models and drug-testing platforms to be one of the most rewarding pursuits in my professional career. I can’t wait to see what this team will be developing over the next five years, and beyond.”
The chips will feature photonic biosensors crafted by Benjamin Miller, a Dean’s Professor of Dermatology at Rochester with joint appointments in biomedical engineering, biochemistry and biophysics, optics, and materials science. Miller, the center’s associate director for resources, says the center is the culmination of years of research and collaboration.
“Getting our devices qualified by the FDA as drug development tools will mean that we’re a step closer to doing ‘clinical trials on chip’ with fully human models, increasing the likelihood of a drug candidate being successful when it actually gets to human clinical trials,” says Miller. “This is also a great opportunity to build an interdisciplinary training environment for our students and expand a collaboration with my colleagues that has been very productive.”
Far-reaching implications
Joan Adamo, director of the Office of Regulatory Support at the University of Rochester Medical Center’s Clinical and Translational Science Institute, will serve as associate director for qualification and will prepare all submissions to the FDA for qualification. Adamo says she sees the ambitious program having far-reaching implications.
“This unique program involves close collaboration with the FDA through a series of qualification steps—a critical aspect to addressing unmet needs,” says Adamo. “I am looking forward to working closely with the agency and our collaborators on this regulatory science project. We will achieve qualification of these vital drug development tools, which will accelerate research conducted at URMC and be shared with other academic health centers and industry programs.”
George Truskey, the R. Eugene and Susie E. Goodson Distinguished Professor of Biomedical Engineering at Duke University, will serve as associate director and direct collaborative activities at Duke University. The TRaCE-bMPS is also supported by a deep network of co-investigators at Rochester, Duke, and Rochester Institute of Technology, a distinguished advisory board, expert consultants, and key industry partners. The NIH grant is expected to fund TRaCE-bMPS through fiscal year 2028 (FY28).







No comments yet