The paper, “Pyrogallol Impairs Staphylococcal Biofilm Formation via Induction of Bacterial Oxidative Stress,” was recently published in the Journal of Applied Microbiology, an Applied Microbiology International publication.
The study was led by UNE alum Katharina Roese, who is a former student researcher for Kristin Burkholder, Ph.D., associate professor and assistant academic director of the School of Biological Sciences, who was the principal investigator on the study.
Reducing biofilm formation
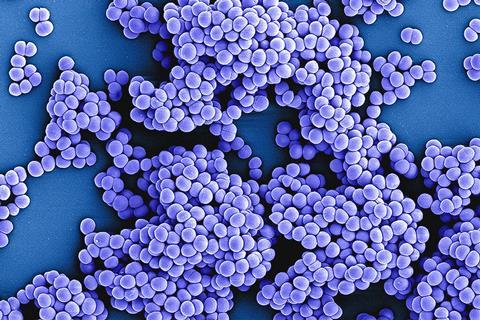
The research team set out to explore methods for reducing biofilm formation for two types of Staphylococcus bacteria that are prone to causing infections in hospitals, notably on in-dwelling medical devices such as catheters or surgical implantations.
The bacteria studied, Staphylococcus aureus and Staphylococcus epidermidis, are among the leading causes of such infections and are notable for their robust ability to form biofilms, which are layers of bacteria trapped in slimy secretion, called an extracellular matrix, that can accumulate on various types of surfaces.
According to Burkholder, biofilms that form inside the body can break off and travel through the bloodstream, attaching themselves to organs like the heart and causing sometimes life-threatening infections.
Testing pyrogallol
Based on available scientific literature, the researchers decided to test the ability of pyrogallol, a phenolic compound used in several clinical applications for its anti-inflammatory effects, to disrupt biofilm formation.
The researchers exposed four strains of Staphylococcus to varying concentrations of pyrogallol. Through observation, the team determined that pyrogallol successfully prevented biofilms from forming in Staphylococcus samples, although the compound did not reduce the prevalence of existing biofilms.
Additional testing revealed that pyrogallol inhibited biofilm formation by causing bacterial oxidative stress, demonstrating — possibly for the first time — that oxidative stress is an effective mechanism in preventing staphylococcal biofilms from forming. Burkholder said this is the most impactful of the group’s findings as it opens doors for research into new treatments that can use oxidative stress to treat and prevent infections.
Broad-spectrum antibiotics
She also said such findings show promise for reducing the need for broad-spectrum antibiotics in hospital settings, which research has suggested may lead to further antibiotic resistance.
“By preventing biofilm formation on in-dwelling medical devices, you may reduce the need for antibiotics in treating biofilm-related infections,” Burkholder said. “Pyrogallol prevents these bacteria from doing what they need to do to cause infection. There are a lot of potential compounds that we can use to treat Staphylococcus in the same way. If we can develop some novel therapeutic that reduces the need for traditional antibiotics, we will reduce the chance for continued emergence of drug-resistant microbes.”
The paper’s publication was the culmination of years of work by Roese, who began her academic journey as a volunteer in Burkholder’s lab at just 17. She then studied in Burkholder’s lab as both an undergraduate and graduate student and used the pyrogallol research for her master’s thesis.





No comments yet