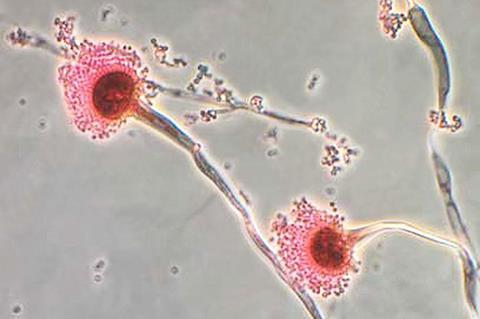
Pulmonary aspergillosis - a group of infectious respiratory diseases caused by various species of the fungus Aspergillus fumigatus - has a significant mortality rate across the globe.
Currently, the first-line antifungal therapy in patients with chronic pulmonary aspergillosis and invasive pulmonary aspergillosis is azoles, which belong to a class of antifungal drugs. However, resistance to azoles in A. fumigatus can result in treatment failure and is a cause for concern.
A recent study published in the journal Microbiology Spectrum demonstrates the synergy of statins, such as pitavastatin (PIT), in combination with azoles against A. fumigatus, even against resistant strains, in a silkworm model.
Statins in vitro
The study was led by Hidetaka Majima, Assistant Professor at the Division of Clinical Research, Medical Mycology Research Center, along with Akira Watanabe and Teppei Arai from the Medical Mycology Research Center and Katsuhiko Kamei from the Japanese Red Cross Ishinomaki Hospital and Medical Mycology Research Center, all affiliated to Chiba University.
“Statins, which are antihyperlipidemic agents, have been reported to have antifungal effects in vitro, but no reports have detected the in vivo antifungal effect against A. fumigatus so far,” explains Dr. Majima.
The team of researchers first obtained various strains of A. fumigatus from clinical isolates and subcultured them. Then, they tested the efficacy of antifungal azoles, like itraconazole (ITC) and voriconazole (VRC), alone and in combination with PIT, against the different strains.
Synergistic effect
Antifungal susceptibility testing was conducted to determine the minimum inhibitory concentrations (MICs) of azoles, i.e., the minimum concentration that is effective against the different strains. Strains with high MICs of ITC or VRC were classified as azole-resistant, while others were considered azole-susceptible.
The interactions between azoles and PIT were evaluated through a checkerboard method, and their interactions were classified as either synergistic, neutral, or antagonistic. In vitro experiments showed a synergistic effect of PIT with ITC against azole-resistant strains, but not against azole-susceptible strains. A similar synergy was observed with VRC for both, azole-resistant as well as -susceptible strains.
Therefore, the researchers focused on the combination of PIT and ITC for further in vivo experiments, where they infected the silkworms with A. fumigatus and administered antifungal drugs 24 hours later. The team examined the survival rates of silkworms infected with an azole-resistant A. fumigatus strain ‘IFM63224’ after treatment with PIT alone, ITC alone, or a combination of PIT and ITC.
They found that the survival rates were better in the combination-therapy (PIT and ITC) group than for the no-treatment and PIT-alone groups but found no significant difference between the combination-therapy and ITC-alone groups.
Interesting lead
However, the results for IFM64301 - a strain of A. fumigatus that had not yet developed any resistance to azole-based drugs - were slightly different. In this case, the combination treatment did not exhibit any synergistic effects when tested in vitro, but the combination group demonstrated extended survival compared to the no-treatment, ITC-alone, and PIT-alone groups in silkworm models.
To further confirm these results, the team conducted a histopathological analysis of the silkworms, which revealed a reduction in fungal infection in silkworms treated with combination therapy as well as ITC alone.
However, the combination therapy showed a unique reduction in the number of fungal hyphae around fat bodies in the silkworms, not seen in the ITC-alone group. This offers an interesting lead regarding the mechanism of action through which PIT might exert antifungal effects.
Combination promising
Taken together, these results demonstrated that the combination of PIT and ITC was effective in combating A. fumigatus infections in the IFM64301 azole-susceptible strain rather than the IFM63224 azole-resistant strain.
“We could detect the in vivo efficacy of pitavastatin combined with azole against A. fumigatus for the first time. As opposed to most statins, PIT barely shows any drug–drug interaction with azoles in humans and can be used safely with ITC. Although the effective dose in silkworm models is higher than the dose of PIT for dyslipidemia in the human body, this result can present a potential new treatment strategy against A. fumigatus in the future,” concludes Dr. Majima.
In summary, although further clinical trials seem warranted, the study results suggest that the combination of PIT with azoles, especially ITC, may be a promising option for effective antifungal treatment of A. fumigatus.





No comments yet