The answer to antimicrobial resistance might not be the continual discovery of new antibiotics - but judicious use of the antibiotics and insights into antibiotic producing organisms we have already discovered.
Many people take it for granted that infections can be easily treated by a short course of antibiotics; but what would happen if the antibiotic discovery pipeline slowed down to a trickle? Surprisingly, this is what happened almost 50 years ago.
Since then physicians have relied on modified versions of older antibiotics to stay one step ahead of antimicrobial resistance. However, modifying peripheral groups of an antibiotic is really only tinkering with the problem and only holds resistance at bay for a limited period of time.

Therefore, one of the main targets of new antibiotic exploration is the discovery of therapeutics with a significantly different core structure that could delay the development of antibiotic resistance. Distressingly, there have been very few new core antibiotic structures discovered since the 1970s.
Of course, it may seem logical to chemically synthesize completely new core antibiotics or significantly modify them. However, this approach has been tried without much success due to unforeseen problems with stability and toxicity of new structures, and perhaps more significantly a low return on investment which caused the majority of major pharmaceutical companies to leave the discovery field.
Going to extremes
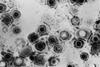
Fortunately, improved access to genetic sequencing has come to the rescue, revealing that antibiotic producing organisms can be detected in extreme environments where it was previously thought that life could not exist. These include places such as deserts, polar regions and hypersaline lakes. It is thought that physiological adaptions to these extreme environments have helped in the discovery of new antibiotics such as chaxamycins, atacamycins and chaxalactins from Atacama desert.
However, new antibiotic discoveries were not only confined to these extremes, but also to ‘shared habitats’ where antibiotic producing organisms live in symbiosis with organisms such as sea sponges to produce nocardiopsistin or with ants to produce attinimicin.
Antibiotic producing organisms such as Streptomyces have also been discovered in association with traditional or historical medicines, which had not previously been appreciated.
More efficient mechanisms
Discoveries of these microorganisms have not only uncovered the identity of new antibiotics but have also revealed more efficient mechanisms of antibiotic production in extreme environments.
For instance , genomic sequencing of a desert Streptomyces violaceusniger strain SPC6 revealed the identity of a new tRNA which overcomes a certain ambiguity in the translation of antibiotic gene clusters which is present in mesophilic species. When this more efficient system is transferred into mesophilic species, it increases antibiotic production and even produces some silent/cryptic antibiotics which are not usually produced under standard conditions.
Some scientists caution that repeating older methods of antibiotic discovery and prescribing these in a conventional manner might just lead to a similar situation of antibiotic resistance to what we have today, albeit over several decades. On a positive note, they add that we probably have enough insights into antibiotic synthesis to tackle the problems of infection and resistance, if we carefully observe their molecular ecology.
Combination therapies
Antibiotics are just one of the many secondary metabolites released at some stage of a microorganism’s lifecycle. Interestingly, many of these additional compounds have been reported to increase the stability and efficacy of antibiotics while ameliorating the development of antibiotic resistance. Indeed it has recently reported that siderophores, iron scavenging compounds, in combination with antibiotics can be used to create a ‘trojan horse’ strategy which tricks the iron transport system of pathogens into delivering antibiotics into their own cells.
Despite the helpful attributes of these adjuvant compounds, modern chemotherapeutic methodologies concentrate on dispensing only one purified compound. However, there are some prescription regimens that already combine several antibiotics together, such as the treatment of tuberculosis. In other cases beta-lactam antibiotics are regularly combined with beta-lactamase resistance blockers such as clavulanic acid, for example Augmentin.
Recent research has confirmed that combinations of several compounds or adjuvants mitigate against the development of AMR (Mattingly et al., 2020). Although these combination strategies might introduce slightly more complex considerations, antibiotic chemotherapy would definitely reap the benefits in the longer term.
This article is adapted from ’Going to extremes: progress in exploring new environments for novel antibiotics’ which has been published in npj antimicrobials and resistance.






No comments yet