As you exhale, hundreds of chemical compounds in your breath are released into the air, including volatile organic compounds (VOCs) - a large group of carbon-based chemicals that can be derived from metabolic processes in the body.
This also encompasses compounds generated by the metabolisms of more than 10,000 microbial species residing within our bodies. Since these compounds essentially reflect the changes in metabolic processes, they provide a snapshot of the physiological state. Human observation of how breath can smell differently in individuals with specific diseases dates back to ancient Greece. In his treatise on breath aroma and diseases, Hippocrates associated a unique breath scent with liver failure, terming it “fetor hepaticus”. However, the processes of identifying specific compounds, their original sources, and their connection to diseases, have only emerged in the last few decades.
Microbial metabolites are a game-changer for disease diagnosis
There has been a keen interest in understanding the gut microbiome in recent years, and several metabolites produced by gut bacteria have been found in different biological substances such as faecal matter, suggesting they impact the physiological condition of the human body.
For example, phenol and p-cresol are substances produced by bacteria when breaking down certain amino acids like tyrosine, which is vital for creating important molecules that play a role in regulating immune, metabolic, and neuronal responses. Short-chain fatty acids (SCFAs), such as butyrate, acetate, and propionate, are thought to regulate blood pressure when bound to G-protein-coupled receptors, a large and diverse family of receptors on the surface of cells that are important for transmitting signals from outside the cell to the inside. These SCFAs come from dietary fibres, which cannot be metabolised by the human body but serve as a good source for fermentation by gut microbes.
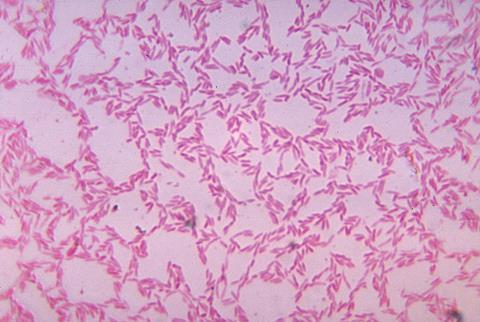
Trimethylamine (TMA), another compound produced from food, is made by gut bacteria when they break down animal-based substances like phosphatidylcholine, choline, and L-carnitine. Studies in humans have connected it to kidney disease and colorectal cancer. TMA is then converted to trimethylamine N-oxide (TMAO) in the liver. TMAO has been linked to increased inflammation and oxidative stress, which are factors implicated in various health conditions. For instance, having a high level of TMAO in the blood has been linked to a higher chance of heart and metabolic issues. In one study, researchers found distinct differences in the gut bacteria of healthy people and those with chronic heart failure, with the decrease of Faecalibacterium prausnitzii and increase of Ruminococcus gnavus being key differences. This highlights the interconnectedness of microbes and their metabolic products with human physiological conditions and their association with diseases.

The capability to detect and determine microbially produced compounds in breath and apply them in clinical settings can bring tremendous benefits in diagnosing and monitoring microbiome-relevant diseases. Breath offers several advantages for biological sample collection compared to other matrices such as blood, urine, and faecal matter. For instance, breath is virtually inexhaustible, making it ideal for repeated sampling within a short timeframe. The sample collection process is non-invasive, painless, and reduces the risk of infection. Unlike urine and faecal matter, breath can be sampled at any time, allowing for nearly real-time reflection of metabolic processes. These numerous benefits have made breath sampling more favourable over other tests. Researchers are working to identify and validate specific VOC biomarkers from exhaled breath, in the hope of using them as a tool for diagnosing diseases and monitoring treatments in clinical settings.
Breath tests are already in use in clinical settings. For example, urea labelled with 13C is used as a metabolic probe to diagnose a Helicobacter pylori infection in the gastrointestinal tract. A more recent successful development in translating breath biomarkers for clinical use are hydrogen methane breath tests (HMBTs), routinely used for diagnosing conditions such as small intestinal bacteria overgrowth (SIBO) and carbohydrate malabsorption (including lactose and fructose intolerance). As these conditions often present with complex and overlapping symptoms, the development of more accurate diagnostics is estimated to benefit over one billion people worldwide. The success of these breath tests in the clinic is encouraging for researchers to identify more volatile compounds and understand how they connect to specific diseases, making breath sampling an important platform to study microbial biomarkers. Meanwhile, companies such as OMED Health are working to make breath testing for gut health issues more accessible to the general public and healthcare professionals.
Exhaled breath contains compounds made in the gastrointestinal tract
As many important compounds related to the microbiome are volatile, analysing breath composition can help detect changes in the gut microbiome. VOCs that are detectable in the breath are those with key properties such as high vapour pressure and a low boiling point, making them gaseous at room temperature. The typical size range of chemicals that can be detected and identified is 50-600 molecular weight (Da) and can span a broad range of chemical classes.
Breath is comprised of volatile compounds with two major origins - those that have been inhaled from the outside air, and those that have arisen from internal processes in the body. This includes human processes such as inflammation from external sources such as diet. However, a large variety of volatile compounds actually stem from the many ongoing metabolic processes of microbes in the gastrointestinal tract.
These volatile compounds can diffuse away from their point of origin into the dense network of blood vessels around the intestines and travel through the bloodstream. Upon reaching the blood vessels in the lungs, the alveolar membrane - the boundary between the outside air and the lung tissue - serves as a launch pad for volatile chemicals, allowing them to be exhaled. Most of the detectable volatile compounds in the breath that are produced from either human or microbial metabolism, stem from blood–air alveolar exchange in this manner.
Importantly, this relationship means that the concentration of volatile compounds in breath is directly related to their concentration in the blood, underpinned by their physicochemical and physiological properties. For an average person, their total blood volume circulates through their lungs approximately every minute, meaning that a breath sample taken over one minute contains compounds that have originated from the entire body - with the gastrointestinal community of microbes producing a significant proportion of them.
Advanced analysis can identify specific compounds in breath
There are many methods to identify and measure the volatile compounds in a breath sample. Gas chromatography-mass spectrometry (GC-MS) is widely accepted as the gold standard due to its versatility and sensitivity. Breath can be collected through various means, such as exhaling into Tedlar bags or specialised breath collection devices. These breath samples are then analysed using a GC-MS system, usually compared to “blank” air samples from the surrounding environment. This approach distinguishes compounds that have been inhaled from those truly originating from the breath.
GC-MS can reliably detect hundreds of biologically relevant compounds in a breath sample, and different types of GC columns can be used and fine-tuned to capture compounds with specific chemical properties. A GC-MS dataset consists of a series of peaks that vary in size and shape depending on the abundance and chemical identity of the compounds, which can be used to identify the compounds in the breath sample for analysis. Some HMBTs employ a GC-MS workflow. Notably, during the COVID-19 pandemic, the FDA emergency-authorised the InspectIR COVID-19 Breathalyzer, a rapid breath test using GC-MS that could identify SARS-CoV-2-associated compounds in less than three minutes – a clear sign of the clinical feasibility of GC-MS breath testing.
Other breath analysis methods such as portable sensor-based devices detect the overall pattern, or “breathprint”, of exhaled breath, rather than separating and identifying the specific compounds in the sample. These techniques have the advantage of increased portability and can be quicker to complete. However, sensor-based approaches come with technical issues such as drift and sensor faults that are not as easy to control. Not identifying what the compounds in breath are can also lead to difficulty in understanding the underlying biology and can impact the consistency of results between studies.

The microbiome-breath-disease relationship provides insights into diagnosis, treatment, and monitoring
To identify potential microbial markers in breath, it is crucial not only to understand where they originate from, but also to uncover the relationships between specific microbes, volatile compounds, and diseases.
Several breath studies have linked specific substances produced by gut bacteria to specific conditions and diseases. In one study on Crohn’s disease (CD), researchers collected breath and faecal samples from individuals during both times of active disease and times of no symptoms. They found that certain VOCs in breath, like acetate and propionate, were closely correlated with the levels of Bifidobacterial and Firmicutes bacteria, for both states. Importantly, the relative abundance of these substances and the correlated microbes were lower when the disease was active. Interestingly, the study also found significant correlations between the VOCs pentane and octane and Bacteroides fragilis and Ruminococcus gnavus in the disease-active state. While these alkanes can be produced as a result of inflammation, this study demonstrated the implicit connection between microbial-produced breath VOCs, gut bacteria, and disease states.
Similarly, a recent study investigated the correlation between exhaled breath VOCs and the bacteria found in stool samples from gastric cancer patients and healthy controls. While the types of gut bacteria did not differ much between patients and controls, a higher number of breath compounds correlated with a higher number of bacterial species in patients than in controls. These VOCs in breath were closely tied to specific bacteria and were unique to each group – there were no common VOCs found in both groups. The findings suggest that there may be different underlying metabolic processes between gastric cancer patients and healthy controls, and that studying the link between breath VOCs and microbiota could help improve our understanding of changes related to cancer, which could lead to better outcomes and longer lives for those affected.
Ethanol breath tests could revolutionise liver disease treatment
Another substance made by gut bacteria, ethanol, has long been thought to be only detectable in the breath when alcohol is ingested. However, it could be a game-changer in diagnosing and monitoring liver disease.
Some studies have suggested that microbial dysbiosis may be associated with the development of non-alcoholic fatty acid liver disease (NAFLD) and non-alcoholic steatohepatitis (NASH) through the overproduction of ethanol by certain bacteria, such as Klebsiella pneumoniae. However, because ethanol is broken down by enzymes in the liver before reaching the peripheral circulation, only a slight elevation of circulating blood alcohol was found in the blood of people with these liver diseases compared to healthy people. Interestingly, when these enzymes in the liver are blocked, ethanol levels in the blood going from the gut to the liver were up to 187 times higher in people with NASH. The higher the ethanol, the more severe the liver disease seemed to be. Additionally, when these NASH patients took antibiotics for a week, their levels of ethanol dropped significantly. This indicates that even if people refrain from consuming alcoholic drinks, gut bacteria might already produce enough ethanol to surpass the safe limit for daily consumption in those with NASH.
This discovery could drastically impact the pharmaceutical industry, given that around 40 percent of prescribed medications can potentially interact with alcohol.
Currently, there are at least eight classes of drugs for NASH treatment in development, each acting against different relevant targets to alleviate symptoms or slow disease progression. However, identifying people whose gut bacteria produce ethanol is crucial before starting treatment, as alcohol can interfere with NASH drugs, making higher doses necessary for them to work properly. A diagnostic test for bacterial ethanol production is needed to help identify individuals at risk of high ethanol exposure. This would help in selecting the right patients for drug trials, increasing the chances of desired outcomes, and establishing drug efficacy.
Currently, there is a lack of devices for routinely and non-invasively monitoring the ethanol produced by microbes. Breath levels of ethanol from gut fermentation are expected to be less than 20 ppb (parts per billion), which is below the detection limit of current commercially available breathalysers. These extremely low levels would require lab-based analytical instruments with much more sensitive detection capabilities. However, with further development, this technology could eventually translate into handheld devices for at-home testing.

Studying breath could reveal how gut bacteria influence the brain
An exciting area of emerging research is investigating how the gut microbiome communicates with the brain through a complex network called the microbiota-gut-brain axis. Studies have demonstrated that substances produced by gut bacteria can cross the blood-brain barrier, directly affecting the brain.
Higher levels of one such substance, 4-ethylphenylsulfate (4EPS), have been observed in autism spectrum disorder (ASD) both clinically and pre-clinically. This substance is made from 4-ethylphenol (4EP), a volatile compound produced by gut bacteria and detectable in exhaled breath. When 4EPS enters the brain, it may disrupt the growth of important myelinating cells in the central nervous system. Mice that were bioengineered to produce 4EPS showed more anxiety-like behaviours, and this effect was lessened by drugs that restored the function of myelinating cells. This demonstrates how one microbial-produced metabolite can impact the brain. Gut bacteria produce many metabolites circulating in the body, and the composition of the gut microbiome could influence human cognition. As many of these metabolites or their pre-cursors are volatile, studying breath could help find out more about these compounds that impact the link between the gut, brain, and body.
Breath analysis can support next-generation microbiome research
Breath could also serve as an important new sampling medium to analyse changes in the gut microbiome for clinical and research use. There are many unique benefits of analysing breath. Currently, the method of choice for many microbiome studies is faecal analysis, which has several limitations. Despite containing informative compounds, it reflects a broad period of digestive passage ranging from 10 to 73 hours. Certain microbes are commonly missed in faecal analysis, such as mucosally adherent microbes that are associated with the mucus membrane layer that lines the gastrointestinal tract and those present higher up in the small intestine. Changes in microbial composition can occur across transit that can result in it being misrepresentative. This is important when considering location-specific changes, for example in conditions such as small intestinal bacterial overgrowth (SIBO).
As exhaled breath contains blood-derived compounds, there is no bias for location within the gastrointestinal tract. It is a virtually inexhaustible and continually produced resource, and contains many informative metabolites produced by gut microbiota. Unlike faecal matter sampling, volatile compounds from the gastrointestinal tract are rapidly detectable in the breath after their production, meaning that breath analysis can provide an almost real-time window into the activity of the gut microbiome. A large volume of breath can be collected at any one time, completely non-invasively – the volume of a single exhaled breath at rest is approximately 400-500 mL, with an average of 12 breaths per minute, resulting in about six litres of air being ventilated every minute. This means we can continuously monitor changes in breath composition over time at rapid intervals, which is useful for longitudinal studies.
Breath analysis can also be coupled with innovative approaches like EVOC (exogenous volatile organic compound) probes. An EVOC probe uses a similar rationale to H. pylori and HMBTs, in that they evoke a response from a particular pathway of interest, and is already proving to be a promising approach toward the development of a breath test capable of diagnosing liver disease early. Breath analysis is useful in studies to track changes in gut-microbiota-produced compounds like SCFAs when diets or medications change, or when comparing health and illness or different age groups. The foundational understanding of the relationship between VOCs and microbial metabolism, developed through studies on faeces, blood, and urine, can help design new studies using breath analysis. This can be combined with other, more common types of sample analysis as part of a multiomic approach for increased study strength.
We are still at the beginning of appreciating the multitude of roles that the gut microbiome plays in the maintenance of our health and the development of disease. Breath analysis remains an underutilised tool in clinical research and practice, with immense potential to enhance our understanding of the gut microbiome.
Related reading on The Microbiologist The scent of infection: how smells can help us spot disease.








No comments yet