Zoonotic spillovers have become a significant focus of global health, with outbreaks like SARS and COVID-19 underscoring how quickly these events can escalate into worldwide crises. Researchers lean heavily on genome sequencing to get ahead of the next pandemic. It is a powerful tool for tracing a pathogen’s origin, understanding how it crosses species barriers, and mapping its evolutionary history.
Scientists can spot key mutations and pinpoint the animal hosts involved by decoding and comparing the genetic makeup of viruses, bacteria, and other microbes in animals and humans. This genomic insight helps confirm how a spillover happened and reveals how pathogens adapt to new hosts over time. It is an essential step toward better risk assessment and outbreak prevention.
Genomic surveillance as a forensic tool
Whole-genome sequencing (WGS) and metagenomic analysis have become essential in the hunt for emerging pathogens, especially those lurking in animals. When scientists analyze samples from infected patients or wildlife, they extract microbial DNA, which is sometimes a mix of genetic material from viruses, bacteria, and other organisms.
WGS reads millions of short DNA fragments simultaneously and then pieces them together to reconstruct the complete genome of a microbe. This process allows researchers to identify known pathogens and spot genetic changes that might explain how the organism has evolved or adapted to a new host.
Metagenomic analysis, however, does not rely on prior knowledge. It scans all genetic material in a sample. It can also detect previously unidentified organisms, which makes it especially useful for surveillance in wildlife, livestock, and environmental samples where many microbes are still unknown.
Researchers turn to a growing number of platforms and global networks to support this work. Sequencing technologies power the data collection, while programs like the Global Virome Project provide frameworks for coordinated pathogen discovery and data sharing. Once sequences are uploaded to public repositories, scientists can compare genetic information from human infections with isolates found in animals.
These genomic comparisons help pinpoint potential spillover events, trace transmission patterns, and identify mutations linked to increased virulence or host switching. WGS and metagenomics offer a powerful lens for understanding pathogen evolution and strengthening early-warning systems.

Phylogenetic mapping of cross-species transmission
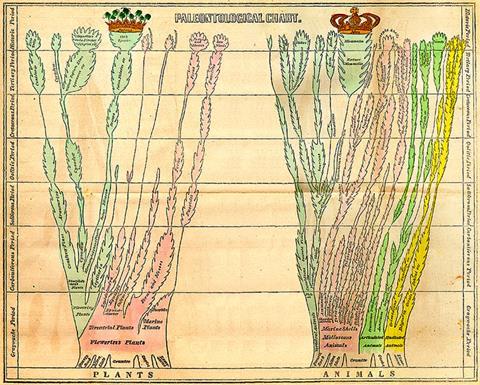
Phylogenetics allows scientists to reconstruct how pathogens evolve and spread by analyzing genetic relationships across samples from different hosts and locations. Comparing slight variations in the genetic code can build evolutionary trees that reveal how a virus or bacterium has changed over time — and, in some cases, jumped from animals to humans.
Tools like BEAST and IQ-TREE can generate time-scaled phylogenies, which estimate when divergence events occurred and help clarify the transmission direction. These methods have been instrumental in tracing the origins of major zoonotic outbreaks.
While phylogenetic techniques can outline transmission chains and identify viral ancestors, they have limitations, especially at the individual level. Researchers caution against using phylogenetics to determine who infected whom in specific cases — like forensic investigations — because the resolution is not always definitive.
However, these methods can still yield valuable insights at the population level. Confidence in source attribution improves when multiple sequences, epidemiological data, and contextual clues are included. When applied carefully, phylogenetics offers a powerful window into the evolutionary history of pathogens and the dynamics of zoonotic events.
Host adaptation and mutational signatures
Genomics gives researchers a front-row seat to watch how pathogens evolve to infect new hosts, especially during zoonotic spillovers. By comparing genome sequences across different species, scientists can identify specific mutations that help a pathogen adapt to human biology. These changes often occur in regions that control how the microbe enters host cells, such as viral surface proteins.
For instance, in influenza viruses, shifts in the hemagglutinin protein allow them to recognize and bind to human receptors rather than their avian sialic acid counterparts. These genetic tweaks may seem small, but they are crucial in determining whether a pathogen can spread efficiently from animals to humans.
Researchers pair genomic analysis with structural prediction tools to understand the full impact of these mutations. This approach reveals whether a new variant is likely to latch onto human cells more effectively or evade the immune system. Structural insights validate genomic findings and help forecast which mutations pose a higher risk for future outbreaks. Combining sequence data with molecular modeling allows scientists to stay ahead of pathogen adaptation, which gives public health systems more time to respond.
Comparative genomics across reservoirs and intermediate hosts
Comparing pathogen genomes across species like bats, civets, camels, and pigs helps scientists identify the original reservoirs and the amplifying hosts that bridge the gap to humans. These cross-species comparisons allow researchers to trace how pathogens evolve and adapt, revealing which animals are most likely to support replication and transmission.
Scientists can uncover the genetic signatures influencing host range and transmission efficiency by analyzing genomic similarities and differences across these animal hosts. This research predicts where the subsequent spillover might occur and prepares surveillance strategies accordingly.
To deepen these insights, researchers turn to pangenomic analysis. This process compares multiple genomes within a species or group and identifies conserved genes that support survival in various hosts and variable regions, driving host-specific adaptation. These variable genomic hot spots often contain clues about receptor usage, immune evasion, or tissue tropism.
Alongside zoonotic viruses, scientists also examine how non-infectious threats like mycotoxins enter the food chain. Mycotoxins affect a quarter of the world’s crops, and livestock that consume contaminated feed can pass these harmful compounds on through meat, milk, eggs, and other animal products. While not pathogens, these toxins highlight the interconnectedness of animal health, food safety, and public risk.

Molecular clock dating and spillover timelines
Molecular clock models help scientists estimate when a pathogen jumped from one species to another by analyzing the rate at which its genetic material accumulates mutations over time. Researchers can calculate the approximate time of divergence and build a timeline of events by comparing sequences from different points in an outbreak or other hosts.
These models rely on the idea that DNA, RNA, or protein sequences change at a relatively constant rate, acting like a genetic stopwatch. When calibrated correctly, molecular clocks can shed light on the timing of spillover events, revealing whether a pathogen circulated unnoticed in animal or human populations before detection.
The accuracy of molecular clock models depends heavily on several factors. One key limitation is that mutation rates are not always as steady as they seem. Some genetic regions may change at a smooth average rate. However, there can be bursts of rapid evolution or periods of stability, especially under selective pressure or across different hosts.
Factors like host immune response, replication speed, and environmental conditions can all influence mutation rates. Calibration also requires reliable reference points — such as well-dated samples or fossil records — which aren’t always available in zoonotic outbreaks. As a result, while molecular clocks offer insights into pathogen evolution and spillover timing, their estimates should be interpreted cautiously and supported by other lines of evidence.

Challenges in zoonotic genomics
Even with the growth of genomic technologies, there are still significant challenges in predicting and preventing zoonotic outbreaks. One of the biggest issues is incomplete wildlife sampling. Many species haven’t been sequenced, especially in remote or biodiversity-rich regions. This leaves critical gaps in understanding how pathogens circulate in nature.
Metagenomic data can also be noisy, with contamination from host DNA, lab reagents, or unrelated microbes complicating the analysis. Add the lack of baseline genetic data for many animals and their microbiomes, and it becomes much harder to identify which microbes pose a real zoonotic risk. While genome sequencing can reveal much, these limitations mean it cannot provide a complete picture.
In fact, 60% of emerging infectious diseases come from animals, and about 70% of those go back to wild species. However, studying these pathogens in the field is difficult. Researchers face ethical and logistical hurdles, from safely handling wildlife to operating in challenging environments with limited infrastructure. Cross-border data sharing can also get tangled in policy restrictions or intellectual property concerns, slowing responses to fast-moving threats.
To get ahead of the next outbreak, scientists need better predictive models that factor in mutation rates, protein structures, and ecological behavior. Stronger collaboration and wider data access are crucial to turning genomic insight into real-world protection.

Future directions and innovations
New technologies in zoonotic research promise faster detection and smarter prediction models. AI-driven platforms lead the charge by analyzing massive datasets that combine pathogen genomes, host health records, and environmental data to forecast outbreaks and spot risky transmission patterns before they escalate. These machine learning models identify subtle patterns across species and ecosystems that traditional methods might miss.
Alongside these technologies, researchers combine genomics with proteomics, transcriptomics, and host-pathogen interaction studies to get a fuller picture of how zoonotic pathogens operate. These cross-disciplinary efforts allow scientists to connect genetic changes to real-world behavior, such as immune response evasion or tissue targeting.
Genomics must be at the core of zoonotic disease preparedness
Genomics is crucial in tracing the origins and predicting the emergence of zoonotic threats. For microbiologists, genomic tools offer unmatched clarity in understanding how pathogens cross species and spread. Embracing these methods as part of outbreak preparedness and response plans will be key to staying ahead of the next global health challenge.







No comments yet