Microbiology offers valuable insights into the complex relationship between gut health and mental disorders, revealing how the gut microbiome influences psychiatric conditions such as anxiety, depression, and schizophrenia. By understanding these interactions, microbiological research paves the way for innovative treatments that target gut health to improve mental well-being.
Applied Microbiology International members have free access to the Headspace app. Become a member today.
An overview of the gut microbiota and mental health
Recent studies on the gut microbiome have unveiled its significant role in various psychiatric disorders, including bipolar disorder, schizophrenia, stress, anxiety, and the functioning of reward and resilience systems in mental health. The intricate relationship between gut health and mental well-being has garnered considerable attention in scientific research and clinical practice.
One of the most fascinating findings is the association between gut microbiota and schizophrenia. Research indicates that individuals with schizophrenia often exhibit altered gut microbiomes compared to healthy controls. For instance, certain bacteria that produce neurotransmitters, like serotonin and gamma-aminobutyric acid (GABA), show reduced abundance in those with schizophrenia thus suggesting a link between gut microbiota and central nervous system disorders, including schizophrenia. This could contribute to the disorder’s symptoms, as these neurotransmitters play a crucial role in regulating mood and cognitive functions.
There have also been instances where probiotics and dietary changes aimed at modulating the gut microbiome have shown promise in alleviating some psychiatric symptoms like depression, cognition, and emotion. In a current unpublished bibliometric analysis by myself and colleagues at Poznan University of Medical Sciences exploring research trends on the intersection of antimicrobial resistance and mental illness, we found the major connector to be the gut microbiome.
Stress and gut health
Stress and anxiety also demonstrate a compelling link to gut health. The gut-brain axis – a bidirectional communication pathway between the gut and the brain – plays a pivotal role here. Chronic stress levels can lead to dysbiosis, an imbalance of gut bacteria, which in turn can exacerbate feelings of anxiety and stress. For example, studies have shown that individuals under chronic stress may have increased levels of inflammatory markers, which can affect not just gut function but also mood regulation. Conversely, probiotics such as Lactobacillus and Bifidobacterium species have been explored as a potential treatment avenue, with some studies suggesting they can reduce anxiety symptoms by promoting a healthier gut microbiome.
The gut microbiome influence on reward and resilience systems
The gut microbiome’s influence on reward and resilience systems adds another layer to understanding mental disorders. The microbiome can affect the brain’s reward pathways, which are often dysregulated in conditions like depression and substance use disorders. Certain bacteria metabolise compounds that influence dopamine levels, which are critical for mood, motivation, and reward processing. For instance, research shows that specific strains of Lactobacillus, such as Lactobacillus helveticus and Lactobacillus fermentum NMCC-14, could enhance dopamine production, potentially impacting mood and the brain’s reward responses. Resilience to stress and coping with adversity has also been linked to gut health. Those with a more diverse gut microbiome tend to show greater psychological resilience. This diversity is crucial because a varied gut environment is more likely to produce beneficial metabolites that can influence emotional regulation and stress responses.
The influence of food insecurity on the gut microbiome and mental health
Food insecurity, especially linked to microbial contamination, has substantial implications for mental well-being, stress levels, and anxiety. When individuals face food insecurity, they often have limited access to safe, nutritious food, which can result in increased reliance on processed or contaminated foods. This not only affects physical health but also significantly impacts mental health, particularly in vulnerable populations such as children and adolescents, critical periods for neurodevelopment.
In our recent study led by Ovinuchi Ejiohuo (Poznan University of Medical Sciences) and Dr Helen Onyeaka (University of Birmingham), we show an interconnection between food insecurity and heightened stress and anxiety. This chronic stress can lead to altered gut health, as anxiety and stress can contribute to dysbiosis. This can impair neurodevelopment in children and increase susceptibility to psychiatric disorders later in life. For instance, we highlighted in our review that children in food-insecure households are more likely to experience symptoms of depression and anxiety. Additionally, these stressors can compromise immune function, making individuals more vulnerable to infections and further disrupting gut health. This cyclical relationship emphasises the importance of ensuring access to safe and nutritious food to foster physical and mental health.
Microbial contamination of food can exacerbate these issues. Foods contaminated with pathogens like Escherichia coli, Salmonella, or Listeria can lead to foodborne illnesses, adding to physical stress and health anxiety. For instance, a foodborne outbreak might lead to not only physical illness but also emotional distress, further impacting overall mental well-being. The mental burden associated with dealing with food-related illnesses can lead to a heightened state of anxiety, especially in individuals already struggling with mental health issues.

To combat these challenges, food microbiology methods can be instrumental in sourcing sustainable foods and developing food supplements that support mental health. Researchers can identify beneficial microbes that promote gut health by applying advanced microbiological techniques such as high-throughput culturing, the roll tube method, metagenomic sequencing, and proteomic and metabonomic analysis.
Specific strains of bacteria, such as Lactobacillus and Bifidobacterium, can be isolated and studied for their ability to enhance gut health and, consequently, mental well-being. This can lead to the development of functional foods that provide additional health benefits beyond basic nutrition. Probiotics derived from fermented foods like yoghurt, kefir, and kimchi have been shown to influence the gut microbiome positively. They can help restore gut balance, reduce inflammation, and even modulate neurotransmitter production, improving mood and cognitive function. Also, utilising sustainable agricultural practices can help ensure the safe production of these foods, minimising contamination risks. For instance, bio-control methods such as certain beneficial bacteria, yeasts, and phage can reduce the incidence of pathogenic microbes in crops, thus enhancing food safety.
Dietary supplements designed to support gut health specifically offer another avenue for managing psychiatric disorders. Omega-3 fatty acids, amino acid precursors like L-tryptophan, and vitamins such as B12 have been linked to better mental health outcomes. Integrating these supplements into treatment plans can help bolster the gut microbiome and provide additional nutrients necessary for optimal brain function.
Influence of the gut microbiota on mental disorder candidate genes
A study by Lai et al. 2021 shows that the gut microbiota influences the expression of TRANK1 (Tetratricopeptide repeat and ankyrin repeat containing 1) in patients with bipolar disorder depression by triggering neuroinflammation. This, in turn, affects brain functions such as dendritic spine development and synaptic integrity, contributing to bipolar disorder pathophysiology.
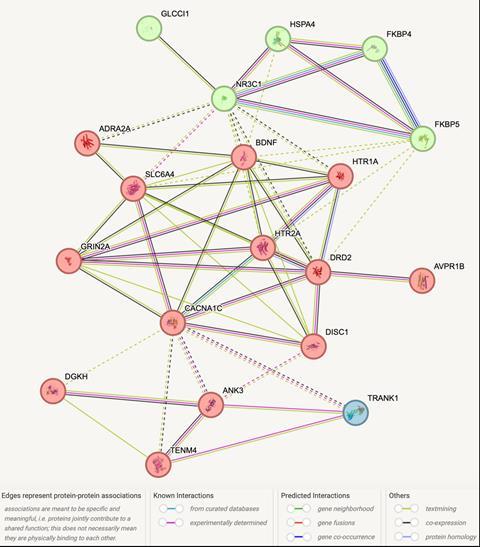
Further insight can be obtained on how TRANK1 links to stress and bipolar disorder by analysing mental disorder candidate gene information. Some of the work we do in our group, led by Prof. Dr. hab. Aleksandra Szczepankiewicz (Poznan University of Medical Sciences), and Assoc. Prof. Dr. hab. Joanna Pawlak (Poznan University of Medical Sciences) involves the exploration of candidate genes in mental disorders, sometimes employing bioinformatics methods. For instance, using the STRING database, we can combine proteins from genes of bipolar disorder and stress, including proteins from candidate genes on ‘The implication of ADRA2A and AVPRIB gene variants in the aetiology of stress-related bipolar disorder’ with TRANK1 protein.. The protein-protein interaction network (Figure 1) shows that TRANK1 protein directly interacts with Teneurin-4, which is implicated in neuronal development and synaptic function; CACNA1C, implicated in calcium channel dysregulation in bipolar disorder and schizophrenia; and Ankyrin-3 protein, whose dysregulation may disrupt neuronal signalling. All of which contribute to the susceptibility to psychiatric disorders.
Microbes as potential drug candidates in treating psychiatric disorders
Microbes play a pivotal role in producing metabolites that can be promising drug candidates for treating psychiatric disorders, such as with the synthesis of neurotransmitters like serotonin and GABA by gut microbiota, which are crucial for regulating mood and anxiety. Therapeutics that enhance the activity of these metabolites could offer new avenues for treatment. Emerging research suggests that microbiome profiling could be used to tailor treatment plans for individuals based on their unique microbial composition. This personalized approach may allow for more effective and targeted therapies in managing psychiatric disorders.
As our understanding of the relationship between gut microbiota and mental health continues to evolve, it opens up exciting possibilities for developing novel interventions that leverage the power of microbes in promoting psychological well-being. Overall, the potential for using microbial metabolites as therapeutic agents represents a promising frontier in psychiatric medicine, providing hope for more effective treatments for those affected by mental health challenges.
Impact of antibiotics on mental health
Additionally, ongoing studies are essential to examine the impact of antibiotics and microbial disease outbreaks, such as mpox and COVID-19, on mental health. Research indicates that antibiotic use can disrupt the gut microbiome, potentially leading to mental health issues like anxiety and depression. For example, patients recovering from COVID-19 have reported heightened anxiety and mood disorders, highlighting the need for comprehensive mental health assessments during and post-infection.
Microbes, mental health, and pharmacological interventions
Insights gained from microbial interactions and mental health can also inform vaccine development. Vaccines must consider not only the biological aspects but also the psychosocial effects on communities. For example, public hesitancy toward vaccines can be influenced by mental health status and is critical to address to ensure widespread acceptance and efficacy. Combining microbiological research with psychological insights can enhance the overall approach to mental health in the context of infectious diseases and vaccinations.
There is ongoing research on immunological responses to microbial antigens that could lead to changes in neurotransmitter levels or reductions in inflammation, both of which play vital roles in psychiatric disorders. This innovative approach could offer new preventative strategies or adjunct therapies for conditions like depression and anxiety, moving beyond traditional pharmacological treatments.
Conclusion
Microbiology offers promising avenues for psychiatry by revealing the significant influence of the gut microbiome on mental health. Interventions targeting gut health could lead to innovative treatments, particularly in conditions like anxiety, depression, schizophrenia, and bipolar disorder. By examining the roles of specific bacteria and microbial metabolites, scientists are discovering ways to enhance mood regulation and cognitive function. Understanding the impact of factors like food insecurity and chronic stress on gut microbiota underscores the importance of holistic approaches to mental health. Targeting the gut-brain axis through probiotics, dietary interventions, and microbial metabolite-based therapeutics will provide innovative, personalized treatments to improve mental well-being and resilience to stress. Overall, advancing microbiological research holds promise for developing personalized therapies that could significantly improve outcomes for individuals facing mental health challenges.
Applied Microbiology International members have free access to the Headspace app. Become a member today.








No comments yet