Consistently high vaccination rates and global health surveillance programmes have helped eliminate poliomyelitis (polio) in almost all countries of the world, except Afghanistan and Pakistan. Yet non-polio enteroviruses can also lead to the same devastating symptoms of ‘acute flaccid paralysis’ (AFP), but the world is lacking formal surveillance systems to trace and control these viruses with paralytic potential.
In a presentation at this year’s ESCMID Global Congress (formerly ECCMID) (Barcelona 27-30 April), Prof Thea Kølsen Fischer, Nordsjællands Hospital & University of Copenhagen, Denmark will highlight the continuous dangers that polio and the other enteroviruses pose and the efforts she and colleagues across Europe have made in setting up a new network in 2017 - ‘European Non-Polio Enterovirus Network’ (ENPEN) – to understand the burden of enteroviruses causing severe disease including polio-like paralysis.
Polio elimination
There is much to celebrate about the story of polio elimination. For example, WHO estimates without the 10 billion or so oral poilo vaccines given over the last decade, some 6.5 million children could today be living with polio-induced AFP.
But even though the European Region was declared polio-free in 2002 detection of AFP cases due to poliovirus still occurs and as recent as 2022 and 2023 two AFP cases due to poliovirus and 6 asymptomatic poliovirus positive cases were found in Israel, while in London vaccine-derived polio virus genetically linked to strains detected in the US and Israel was detected in environmental sampling in 2022.
This prompted a supplementary vaccination campaign in infected areas. Prof Fischer says: “These events highlight the potential for international spread of polioviruses, including in European countries in areas with low vaccine coverage, where the threat of polio has almost been forgotten.”
Poliovirus cousins
Most countries with well-developed surveillance systems will test all AFP cases for poliovirus, and/or test for poliovirus in cases of non-bacterial meningitis. Some also test sewage systems periodically, as happened with the UK detection above. However, these tests rarely reveal poliovirus, and in these high-income settings, it is almost always in the form of vaccine-derived polioviruses. In the WHO Europe region across the decade 2014-2023 a total of 25687 AFP cases were reported, of which 741 contained vaccine derived polio, mostly in Russia, Ukraine and Turkey, respectively.
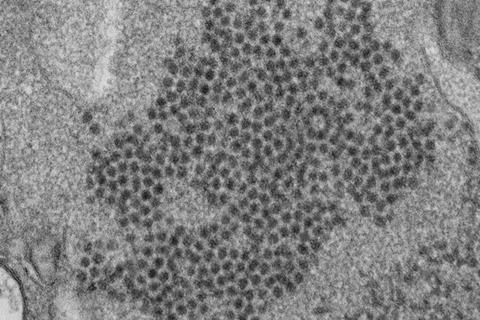
Concerned about the lack of valid data on the burden of non-polio enteroviruses, Prof Fischer and her colleagues in the ENPEN network have been investigating the circulation of paralytic enteroviruses in Europe including enterovirus D68 and enterovirus A71 and documented the circulation of these “poliovirus cousins” in all countries where they have looked.
Their investigations suggest genetic changes in the EVD68 virus is likely one of the explanations to the increased virulence and increased presence of this virus during the past decade. In a recent study from the UK using biobanked blood samples from two decades, Dr Heli Harvala (University College London, UK) who is also a cofounder of the ENPEN network, documented how the seroprevalence of D68 is increasing over time in all age groups.
Sudden onset of paralysis
“Patients can enter hospital with severe respiratory symptoms, but a week after the respiratory symptoms have passed then sudden onset of paralysis can be seen and enterovirus D68 can end up as much more than just a cold,” explains Prof Fischer, although early in its progression the symptoms can be similar.
“Sadly in significant numbers of cases, these infections are progressing to serious complications including lasting paralysis. Yet we have this huge asymmetry in Global Health Programmes, polio having strong surveillance and vaccination programmes. Yet non-polio enteroviruses have neither. Because we don’t have well developed surveillance in place, we can’t say for sure what proportion of these enterovirus infections are leading to serious complications.”
Surveillance is needed
Within the poliovirus surveillance programmes, the clinical cases with CNS symptoms and the AFP cases can see non-polio enteroviruses detected, but analysis is usually incomplete and merely as a by-product as the enterovirus positive samples are usually not further tested into subtypes. “When a child suffers from paralysis, to them and their family it doesn’t matter whether it’s actual polio or another enterovirus that has caused it. We need to get proper surveillance systems in place and work on vaccines for these dangerous non-polio enteroviruses.”
She concludes: “Polio is still a concern in 2024, even in the USA and Europe, and until fully eradicated, it always will be. We must never take our eyes off it and assume it has been dealt with forever. Yet, there is this growing threat of non-polio enteroviruses of which the public and health authorities seem so much less aware. Effective vaccines can be used to eradicate polio. Yet there is no cure, and no vaccines against the paralytic non-polio enteroviruses. We must set up surveillance systems so that all patients who experience acute flaccid paralysis are routinely tested for these enteroviruses. Only then can we identify the scale of the threat, and begin working on preventive interventions like vaccines.”







No comments yet