The bacteria present in the intestine provide information about the quantities of fungi of the potentially disease-causing Candida genus - among them, surprisingly, are lactic acid bacteria that are known for their protective effect against fungal infections.
The findings of researchers at the Leibniz Institute for Natural Product Research and Infection Biology (Leibniz-HKI) and their collaborative partners from Denmark and Hungary add another piece to the puzzle of understanding the human gut microbiome.
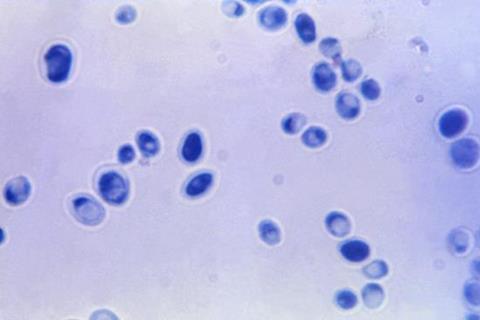
The human gut microbiome is an extremely complex community in which different microorganisms keep each other in check. However, if an imbalance occurs due to antibiotics or other environmental influences, individual species can spread and lead to infection. Fungi of the Candida genus, for example, are present in the intestines of many healthy people. They are usually harmless, but can also cause dangerous systemic infections.
Studying these interactions in the intestine is difficult. The several hundred species of bacteria and fungi can only be partially cultivated in the laboratory, and many are not even known. Researchers at the Leibniz-HKI are therefore trying to shed more light on the intestine using metagenome studies.
Cancer patients
For the study now published in Nature Communications, the researchers examined stool samples from 75 cancer patients and found that certain bacterial species always appear in greater numbers when the amount of fungi from the Candida genus is also high.
“With these data, we developed a computer model that was able to predict the amount of Candida in another group of patients with an accuracy of about 80 per cent based on bacterial species and amounts alone,” explains Bastian Seelbinder, lead author of the study. These bacteria included mainly oxygen-tolerant species.
Seelbinder conducts research in Gianni Panagiotou’s Microbiome Dynamics department at Leibniz-HKI, which focuses intensively on the gut microbiome. What surprised the researchers was not only how successful the prediction of the amount of fungi based on the bacterial species present was, but also which bacteria correlated with high amounts of fungi.
“We found an increased number of bacterial species that produce lactic acid, including Lactobacillus species,” Seelbinder explains. It’s a finding he had not expected. “I could hardly believe it at first, so I checked several times, always with the same result.”
Complexity of microbiome
The reason for his surprise: Several studies have attested to the protective effect of lactic acid bacteria against fungal infections. One of them was published last year by Panagiotou’s group, also in the journal Nature Communications.
“The result shows once again how complex the human gut microbiome is and how difficult it is to decipher the interactions of different microorganisms,” Panagiotou says.
The researchers’ hunch is that lactic acid bacteria, particularly of the genus Lactobacillus, favour Candida proliferation but at the same time make the fungus less virulent.
This could be due to the fact that Candida species can switch their metabolism to be able to use the lactate produced by lactic acid bacteria. This gives them a competitive advantage over other fungi such as Saccharomyces cerevisiae, as the researchers discovered in additional experiments. However, the metabolic switch also apparently causes Candida to remain in its usually harmless spherical yeast form instead of forming fungal hyphae that could invade the intestinal mucosa.
High-risk patients
“There is also a suggestion that certain groups of Lactobacillus species might have different effects,” Seelbinder says. To investigate this, the next step will be to perform more detailed genomic analyses of the bacteria.
“For the current study, we examined stool samples from cancer patients who are particularly at risk for fungal infections,” Panagiotou explains. For further studies, samples from healthy subjects could be included to develop long-term strategies for at-risk patients based on their microbiome.
For their studies, the Leibniz-HKI researchers cooperated with teams from the Korányi National Institute of Pulmonology in Hungary, the Technical University of Denmark and Jena University Hospital, among others.
The study was supported, among others, by the Deutsche Forschungsgemeinschaft (German Research Foundation, DFG) within the framework of the Collaborative Research Center FungiNet (Transregio) and the Cluster of Excellence Balance of the Microverse, as well as by the Novo Nordisk Foundation and the Hungarian National Research, Development and Innovation Office.
Topics
- Bacteria
- Bastian Seelbinder
- Cancer Microbiology
- Candida
- Fungi
- Gianni Panagiotou
- Gut Microbiome
- Jena University Hospital
- Korányi National Institute of Pulmonology
- lactobacilli
- Leibniz Institute for Natural Product Research and Infection Biology
- One Health
- Research News
- Technical University of Denmark
- UK & Rest of Europe





No comments yet