Nirsevimab, a monoclonal antibody, is highly effective in real-world conditions at preventing severe respiratory syncytial virus (RSV) infections in infants, suggests a meta-analysis published in The Lancet Child & Adolescent Health journal.
RSV is a leading cause of serious respiratory illness in young children particularly in the first six months of life, responsible for millions of hospitalisations of children around the world every year. After successful clinical trials, nirsevimab was approved by several regulatory agencies in 2023 and national programmes to provide infants with the monoclonal antibody injection have since been implemented in several high-income countries. This study confirms that the reduction in rates of severe RSV infections observed in clinical trials of nirsevimab can also be achieved in national rollouts of the antibody injection.
READ MORE: Real life data reveals success in controlling respiratory syncytial virus
READ MORE: Why some kids get sicker: The hidden power of nose bacteria
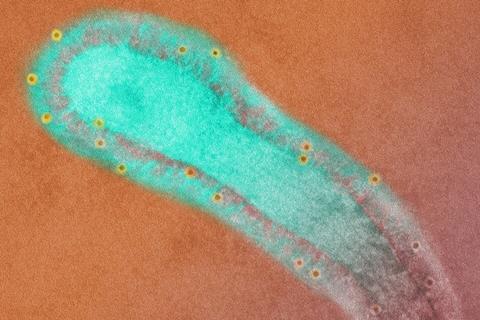
It’s important to note that nirsevimab is not a vaccine despite being delivered as an injection. Monoclonal antibodies are proteins developed in a laboratory that mimic the immune system’s ability to fight off harmful viruses, whereas vaccines prompt the body’s immune system to produce an immune response itself.
Studies across five countries
The meta-analysis of 27 studies conducted during the 2023-2024 RSV season across five countries (France, Italy, Luxembourg, Spain, United States) found on average that nirsevimab reduces the risk of hospitalisation due to RSV infection by 83%, intensive care admissions by 81%, and instances of lower respiratory tract infections by 75% in children aged 12 months and younger. Nirsevimab was associated with higher effectiveness in preventing RSV-related hospitalisation in infants older than 3 months (81%) compared to those aged 3 months or younger (76%).
The analysis also found the effectiveness of nirsevimab for RSV-related hospitalisation varied by country, with higher effectiveness in the US (93%) than in Spain (83%) and France (76%). Authors suggest this may be due to a higher proportion of infants at high risk of severe disease receiving nirsevimab in the US, as these infants were prioritised during the 2023-2024 RSV season due to a limited supply of nirsevimab in the US. However, this theory requires further investigation.
The authors say their findings support the use of nirsevimab as a critical intervention for preventing RSV disease and severe outcomes among infants. However, they caution that the included studies were observational, which may introduce bias due to potential factors such as underlying health conditions, socioeconomic status, or regional differences in healthcare access.






No comments yet