A new assessment of monkeypox infections in a remote area of the Democratic Republic of the Congo (DRC)—with a strain linked to more severe disease than what’s circulating internationally —shows transmission rates rising closer to the point where outbreaks are likely to be larger and more frequent.
The report from researchers at the US Centers for Disease Control and Prevention (CDC), Kinshasa School of Public Health, and the DRC’s Ministry of Public Health is based on data collected between 2013 and 2017, raises fresh concerns about the transmission of monkeypox in Africa.
That includes its potential to cause more cases in African communities, which may in turn increase risks of new outbreaks globally. The findings were presented today at the Annual Meeting of the American Society of Tropical Medicine and Hygiene.
“Our data show that monkeypox transmission in the area we studied was notably higher than previous estimates and was getting close to the point where it can cause large and sustained local outbreaks,” said Kelly Charniga, PhD, MPH, a Prevention Effectiveness Fellow at CDC.
“With today’s interconnected world, outbreaks don’t necessarily stay at their source. This research puts the global health community on alert that there may be the opportunity for larger outbreaks in DRC on the horizon and we must work diligently to prevent future outbreaks where people are most at risk for getting and dying from monkeypox.”
Charniga and her colleagues analyzed reports from 1,463 laboratory-confirmed cases that occurred between 2013 and 2017 in Tshuapa Province in northwestern DRC. The team focused on calculating what is known as the reproduction number, which measures the average number of new cases caused by a single infection.
The effective reproduction number, also known as Rt, is a closely watched parameter for any infectious disease. Rt values greater than 1 indicate that every new infection is causing at least one additional case, with the potential for sustained transmission. Charniga and her colleagues found that the Rt for monkeypox in the region they studied had risen to 0.81. That Rt value is up from 0.3 to 0.5 seen in the 1980s—rates that were consistent with the isolated, sporadic outbreaks of monkeypox that have been occurring in the region for some 50 years.
“When it’s significantly below one, outbreaks die out because fewer people are being infected – and thus spreading the disease to others. That’s what we have typically seen in the DRC, small outbreaks that don’t last,” Charniga said. “But if it gets closer to or above one, then a disease can continue to spread between people in a region and outbreaks can be larger and more frequent.”
The researchers also found new evidence of potentially more regular “spillovers” of monkeypox infections from rodents, which are thought to be the natural reservoirs, to people. Infections from rodents, often involving children, were then continued through person-to-person spread to household contacts. Charniga said that the more this happens, the more opportunities there are for monkeypox to be sustained solely by spread between people.
Monkeypox cases in African countries where the disease has traditionally been found have been increasing during the past several years, including the re-emergence of monkeypox in Nigeria after 40 years with no reported cases there.
“Many people in CDC, the World Health Organization and in health ministries and research institutions across sub-Saharan Africa were calling attention to the rising danger of monkeypox long before we started seeing infections outside of Africa,” said ASTMH President Daniel Bausch, MD, MPH&TM, FASTMH. “This study provides important new insights that point to the urgent need to provide additional resources that can help Africans fight this disease.”
An additional concern is the two different types or “clades” of monkeypox virus. The one that long has been circulating in the DRC—known as Clade I—can have a fatality rate up to 10%, while the fatality rate for the Clade II virus, found in West Africa and the source of recent outbreaks outside Africa, is usually less than 3%. Charniga said severe complications caused by monkeypox, which can include blindness, also appear to be more common with Clade I.
Infections with both clades of monkeypox have become more common in Africa since smallpox vaccination was halted around 1982 following global eradication of the smallpox.
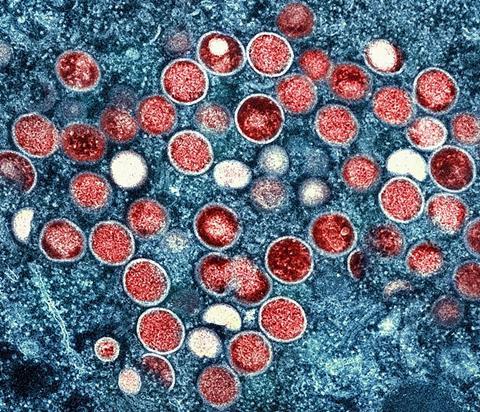
Monkeypox virus is in the same virus family as variola virus, the cause of smallpox, and smallpox vaccines and therapeutics may also work against monkeypox.
However, there is little access anywhere in Africa to these products since most of the global supply was produced as a countermeasure for possible bioterrorism against smallpox and is not widely available. There is now a vaccine licensed for use against monkeypox, but there is only one manufacturer globally and much of its production is under contract to the United States.
Given the poor access to vaccines, fighting monkeypox in Africa—and limiting the risk for new global outbreaks, including those involving the more dangerous Clade I—requires more surveillance and contact tracing to prevent onward spread of monkeypox. Charniga said that since 2010, CDC and the Kinshasa School of Public Health have been assisting DRC with improving surveillance in rural areas, where many clinics still rely on paper forms to report suspected cases.
“The best way to prevent monkeypox from causing more outbreaks in DRC and from becoming a bigger global problem is to devote more attention to areas where it is clearly causing the most suffering today,” she said.
Topics
- American Society of Tropical Medicine and Hygiene
- CDC
- clade
- Democratic Republic of the Congo
- Disease Treatment & Prevention
- Economic Equality
- Infectious Disease
- Kelly Charniga
- Kinshasa School of Public Health
- Middle East & Africa
- Ministry of Public Health
- monkeypox
- Research News
- rodents
- smallpox
- US Centers for Disease Control and Prevention
- USA & Canada
- Virology
- Viruses






No comments yet