The human gut is home to trillions of microbes that not only aid in digestion but also play a key role in shaping our immune system. These microbes communicate with the body by releasing a range of molecules that influence how immune cells grow and function.
To maintain a healthy balance between host defense and microbial coexistence, the body deploys a variety of defense tools—such as mucus, antimicrobial proteins, antibodies, and complement proteins—to control microbial activity and fend off harmful invaders. But one mystery has lingered: Can our bodies selectively recognize and manage specific bacteria among this incredibly diverse microbial community?
READ MORE: Researchers help redefine core microbiome, opening new chapter in precision health
READ MORE: New bacterial product found to inhibit flu virus replication
In a study published in Nature on May 14, a team of researchers investigated this question and uncovered a surprising new way that the body interacts with gut microbes to help maintain intestinal health. This study was led by Prof. Qian Youcun from the Shanghai Institute of Nutrition and Health (SINH) of the Chinese Academy of Sciences (CAS), and Prof. Song Xinyang from the Center for Excellence in Molecular Cell Science of CAS.
Gut lining protein
The researchers began by using advanced protein analysis techniques to compare gut lining samples from germ-free mice and conventional lab mice. This comparison led to the identification of a previously less characterized protein called APOL9, which was much more abundant in regular mice with gut microbes. Further experiments showed that this protein was mainly produced by cells in the intestinal lining.
Then the researchers developed a technique called “APOL9-seq“—a method that combines flow cytometry with genetic sequencing—to identify which bacteria APOL9 binds to. Surprisingly, they found that APOL9—and its human equivalent, APOL2—binds strongly and specifically to a group of bacteria called Bacteroidales, which are common in the gut.
Digging deeper, the researchers discovered that APOL9’s ability to recognize these bacteria depends on a unique fat molecule called ceramide-1-phosphate (Cer1P), which is found on the bacterial surface. When this molecule was removed using gene editing, APOL9 could no longer bind to the bacteria. This study is the first to show that the host can selectively target specific microbes by recognizing their unique lipid signatures.
Outer membrane vesicles
Interestingly, unlike typical antimicrobial proteins that kill bacteria, APOL9 does not harm the microbes it binds to. It causes them to release tiny bubbles called outer membrane vesicles (OMVs)—nanometer-sized sacs filled with bacterial molecules. These OMVs can be taken up by the host’s immune system and used to boost immune readiness. The researchers found that OMVs enhance interferon-gamma (IFN-γ) signaling and increase the amount of MHC-II molecules on intestinal cells. These latter molecules are essential for training a unique group of T cells (CD4+CD8αα+) that help maintain immune balance in the gut.
To better understand APOL9’s role in immune defense, the researchers used a widely accepted mouse model to study the effects of removing the gene. When exposed to Salmonella bacteria, mice lacking APOL9 showed a weaker immune response and more widespread bacterial infection. However, when treated with OMVs derived from the bacteria, these mice displayed stronger immune activity and fewer signs of infection.
Molecular dialogue
“The specific interaction between APOL9 and Cer1P highlights a finely tuned molecular ‘dialogue’ forged through long-term coevolution between the host and its microbiota. In the future, we plan to explore the role of human APOL2 and investigate whether modulating this pathway can strengthen the intestinal immune barrier,” said Prof. QIAN, leading researcher of the study.
This study is the first to show how a host protein can specifically recognize bacterial lipids, thus triggering beneficial immune responses. It also highlights a new way the body actively shapes the gut microbiome—not just by tolerating microbes, but by communicating with them to maintain balance. The findings reveal exciting possibilities for developing next-generation treatments that work by tuning interactions between the microbiota and the immune system.
Topics
- APOL9-seq
- Asia & Oceania
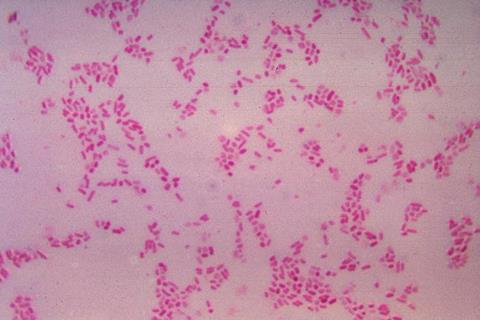
- Bacteria
- bacterial lipids
- Bacteroidales
- Center for Excellence in Molecular Cell Science
- ceramide-1-phosphate
- Gut Microbiome
- Immunology
- Microbiological Methods
- One Health
- outer membrane vesicles
- Proteomics & Enzymology
- Qian Youcun
- Research News
- Salmonella
- Shanghai Institute of Nutrition and Health
- Song Xinyang







No comments yet