A new perspective in Science in One Health examines the World Health Organization’s 2024 Bacterial Priority Pathogens List (WHO BPPL), highlighting its strengths as a research roadmap while identifying critical gaps for a truly holistic antimicrobial resistance (AMR) strategy.
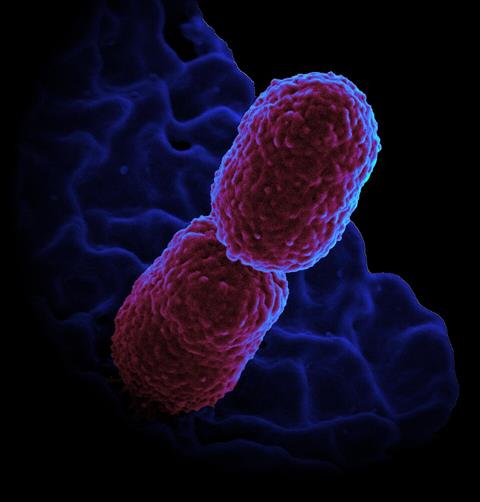
The 2024 WHO BPPL successfully prioritizes 24 antibiotic-resistant bacteria using evidence-based methodology, identifying carbapenem-resistant Klebsiella pneumoniae as the critical-tier threat (84% score). The framework also elevates community-acquired pathogens like fluoroquinolone-resistant Salmonella Typhi and Shigella species to high priority, emphasizing links to inadequate water, sanitation, and hygiene infrastructure.
READ MORE: WHO releases report on state of development of antibacterials
READ MORE: New clinical standards strengthen antimicrobial stewardship in tuberculosis care
Since 2017, at least 13 new antibiotics have been licensed for priority infections, demonstrating tangible progress. The list’s incorporation of preventability metrics also promotes prevention-based strategies, with typhoid conjugate vaccines serving as a proven model for vaccine-focused AMR control.
The One Health gap
However, the analysis reveals a significant limitation: the list’s human-centric focus overlooks critical agricultural and environmental drivers of AMR. Environmental reservoirs of resistance genes in soil, water, and wildlife microbiomes act as amplifiers for human exposure, yet remain underrepresented in global monitoring frameworks. The rise of carbapenem-resistant Enterobacterales, for instance, is often linked to agricultural antimicrobial use—a dimension not captured by current prioritization criteria.
Additionally, surveillance biases toward high-income countries may mask the true AMR burden in low- and middle-income regions, while genetic complexity within priority pathogens—such as high-risk clones of carbapenem-resistant K. pneumoniae (ST11-KLC64)—warrants closer attention.
Call to action
Researchers urge stakeholders to:
· Integrate One Health metrics into future BPPL iterations, incorporating zoonotic risk and environmental spread indicators
· Strengthen global surveillance like the Global Antimicrobial Resistance and Use Surveillance System (GLASS) with equitable data from low- and middle-income countries
· Accelerate therapeutic innovation beyond traditional antibiotics, including bacteriophages, monoclonal antibodies, and vaccine R&D
· Implement antimicrobial stewardship and WASH infrastructure investments, particularly for community-acquired threats
Prioritizing pathogens is not merely a scientific exercise but a moral imperative to safeguard global health equity,. Translating the 2024 WHO BPPL into comprehensive cross-sectoral action is essential to advancing a more equitable and resilient global health response to AMR.
Topics
- Agriculture
- AMR in the Environment
- Antimicrobial Resistance
- antimicrobial stewardship
- Asia & Oceania
- Bacteria
- carbapenem-resistant Enterobacterales
- carbapenem-resistant Klebsiella pneumoniae
- environmental reservoirs
- fluoroquinolone-resistant Salmonella Typhi
- One Health
- Public Health
- Research News
- World Health Organization







No comments yet