New research being presented at the Letters in Applied Microbiology ECS Symposium reveals drive to come up with a better way of diagnosing staph infections that would be more cost-effective and less time-consuming.
Natalie Lamont, a Senior Lecturer and PhD student at the University of Sunderland, is presenting her project ‘Improving diagnostics using MALDI-TOF for the detection of Staphylococcus aureus toxins PVL, TSST-1 and MRSA’.
Staphylococcus aureus is a huge burden on the UK’s health service, as she explains.
Burden on healthcare
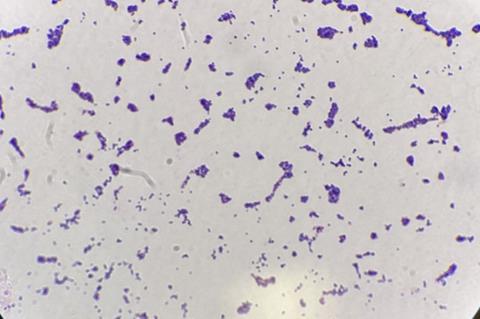
“S. aureus is a Gram-positive bacterium and a common member of human microbiome that can cause a variety of diseases. Infections caused by S. aureus which can possess several virulence factors and resistance mechanisms are current burdens on healthcare, and treatment of skin and soft tissue infections (SSTIs) in the UK,” she says.
“One study estimated a total cost related to acute bacterial skin and soft tissue infections ranged from €1,814.39 to €8,224.06 per patient, while a study in 2021 suggested the cost of PVL S. aureus for inpatients was €2,283, and the cost of treating inpatients with a diagnosis of SSTI caused by PVL S. aureus averaged 5–10 times higher.
“Exotoxins such as Toxic Shock Syndrome Toxin-1 (a superantigen, TSST-1), and cytolysins (haemolysins and leukocidins) such as Panton-Valentine leucocidin (PVL) have key roles in infections caused by S. aureus. “Beta-lactam antibiotics such as Flucloxacillin are the drugs most often selected for the treatment of S. aureus infections. Methicillin was the first penicillinase resistant penicillin and has been widely used in testing susceptibility of S. aureus to penicillinase resistant β-lactam agents.
Resistant strains
“Even though methicillin is no longer available and oxacillin and cefoxitin are now used for susceptibility testing, strains that are resistant to these antibiotics are still known as MRSA. MRSA infections can be harder to treat, associated with increased morbidity and mortality and are a particular concern within hospitals worldwide. Reducing the burden of infection-related mortality is a critical global health objective and WHO includes S. aureus in its priority list of antibiotic resistant pathogenic bacteria that pose a threat to human health.”
In March 2022 the UK case fatality rates for bacteraemia were 22.1% for methicillin sensitive Staphylococcus aureus (MSSA) and 26.3% for MRSA. MRSA infection rates have fallen by around 25% in the past five years but have risen by around 17% for MSSA over the same period: last year there were 3,174 hospital onset cases of MSSA.
Worldwide increase
The prevalence of PVL positive S. aureus has more recently been increasing worldwide, with rates varying between countries. Reported prevalence varies between 13% in China up to 97% in the USA, with the UK reporting 21-46%.
“The frequency of PVL-positive strains differs significantly depending on the population examined; ranging from 1.6% for isolates sent to a reference laboratory for epidemiological typing to 31% for those screened as part of a nationwide sentinel surveillance programme. Reports of infection may not accurately reflect the full burden of PVL since many suspected S. aureus infections linked to PVL are treated without confirmatory testing,” Natalie says.
“According to UK national surveillance data, average toxic shock syndrome S. aureus infection incidence is 0.07 in 100 000 -– however prevalence is again likely not accurately reflected due to lack of testing as treatment is currently mostly based on symptoms.
Rapid detection
“A study in 2021 suggested the cost of PVL S. aureus for inpatients was €2,283, and the cost of treating inpatients with a diagnosis of SSTI caused by PVL S. aureus averaged 5–10 times higher. Effective infection control and rapid detection of these infections could aid in limiting the spread of these kinds of S. aureus infections.
“As a Biomedical Scientist working in an NHS Microbiology department within a large tertiary hospital and trauma centre, it was apparent that identification methods currently used for the detection of S. aureus strains was limited, time consuming and costly.
“Currently, in most NHS microbiology departments S. aureus is cultured on horse blood agar with chromogenic agar used for detection of MRSA, alongside antimicrobial susceptibility testing.
Treatment delays
“These traditional culture methods take 12-48 hours to get a confirmatory result for MRSA, which can result in a delay in treatment and potentially poorer patient outcomes. In recent years there has been a move to rapid molecular analysis for MRSA - however, this is restricted to urgent hospital admissions and locations such as trauma and intensive care only.
“PVL and TSST-1 strains are not routinely tested for following UK standards for microbiology investigation (SMI) guidance, but upon clinicians’ request S. aureus can be sent for further analysis to reference laboratories if these toxins are a concern. Identification is usually performed using molecular analysis or whole genome sequencing for identification of toxigenic strains, which is costly and time consuming.”
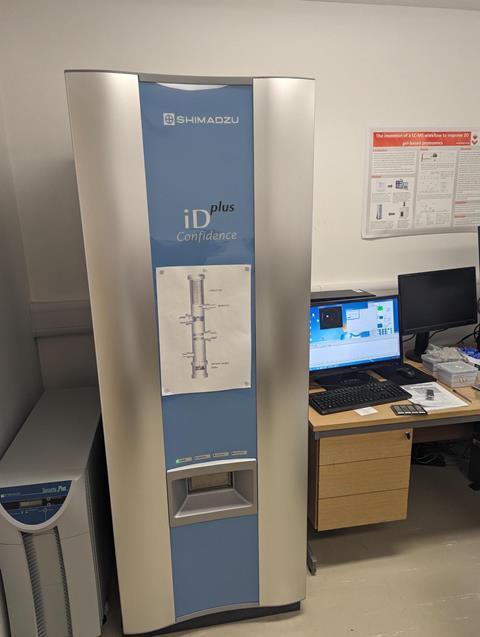
Explaining why she turned her attention to MALDI-TOF, Natalie said it combines two technologies: MALDI for the conversion of the sample into gaseous ions and TOF mass spectrometry for determination of mass-to-charge (m/z) ratios.
Rapid, reproducible, and reliable
“This method compares mass spectra to reference database to identify bacteria and has revolutionised micro-organism identification within the clinical microbiology laboratory, giving an identification in less than an hour. Widespread availability of MALDI-TOF has greatly improved clinical diagnosis of many microbial infections, and it is known for being more rapid, reproducible, and reliable,” she says.
“This study aims to develop novel approaches to detect MRSA and associated toxins (PVL and TSST-1) - specifically, our aim is the detection of PVL, MRSA and TSST-1 in clinical isolates using MALDI-TOF. If successful, these approaches could aid diagnosis, reducing the time to detection, allowing enhanced infection prevention and control measures, and reducing hospital acquired infections.”
Optimal conditions
The first stage was to identify the optimal growth media and conditions for culture of S. aureus to induce the production of the proteins PVL and TSST-1 using a range of culture medium varying aspects that could impact protein production and bacterial growth.
Media investigated so far have included nutrient broth (NB), tryptic soy broth (TSB) and modified CCY medium. Culture protein supernatant was analysed using western blot to determine the level of protein production and preliminary data showed significant differences between media with CCY giving the highest yields of PVL and TSST in supernatant.
The next stage was to process control strain and organisms isolated from patient samples with known MRSA resistance, PVL and TSST-1 protein production on MALDI-TOF from the range of media using multiple sample preparation methods (such as whole cell, partial extraction, full extraction, culture supernatant and protein precipitation) followed by data analysis to determine differences between the various strains.
Data collated to date indicates that full extraction with formic acid for sample preparation improved spectra and gave a higher confidence score when identifying the bacteria and peak analysis in comparison to whole cell analysis.
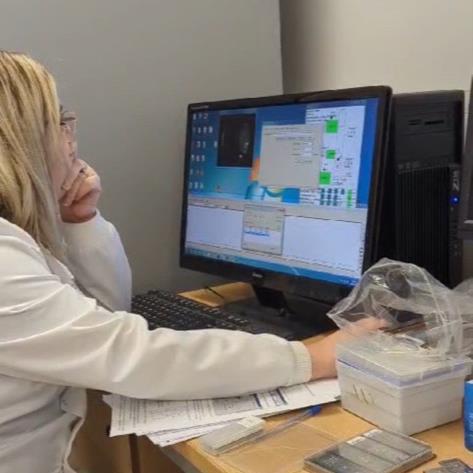
Additionally, MALDI-TOF analysis of CCY supernatant produced improved spectra in comparison to NB and TSB media. When comparing precipitated proteins and culture supernatant there was no significant difference in spectra produced. Further work is required to investigate if MALDI-TOF could be used to differentiate between these strains of S. aureus.
Surprising find
One surprising find was that there has been no difference between the spectra produced from precipitated proteins and supernatant analysis, Natalie says.
“This could be positive news, as it would reduce sample preparation time, removing time consuming steps in the process and reducing cost associated. In the real world this would have a beneficial impact by reducing sample processing time, allowing for faster analysis of S. aureus and aiding in patient management, should the method be utilised in diagnostic laboratories,” she says.
“The next stage of this research is to expand the parameters of m/z range and/or laser intensity on MALDI-TOF, additionally investigate the use of other commercially available matrices could be used and may improve data produced.”
This study was led by Natalie Lamont, supported by Dr Lewis Bingle and Dr Callum Cooper, as part of PhD research, funded by and performed in the University of Sunderland. Anonymised S. aureus isolates were provided by the Microbiology department at James Cook Hospital, Middlesbrough.
The Letters in Applied Microbiology Early Career Scientist Research Symposium will be held at University of the West of England (UWE) in Bristol, UK, on 15 May 2024. To find out more, visit the event page.
Topics
- Antimicrobial Resistance
- Applied Microbiology International
- bacteraemia
- Bacteria
- Callum Cooper
- Clinical & Diagnostics
- Community
- Early Career Research
- Infection Prevention & Control
- James Cook Hospital
- Lewis Bingle
- MALDI-TOF
- Methicillin-resistant Staphylococcus aureus
- Natalie Lamont
- One Health
- Rapid Diagnostics
- Research News
- UK & Rest of Europe
- University of Sunderland





No comments yet