Research led by a University of Maryland scientist in collaboration with the National Institute of Allergy and Infectious Diseases suggests that reducing virulence in drug resistant infections rather than trying to kill bacteria outright may offer an answer to antimicrobial resistance.
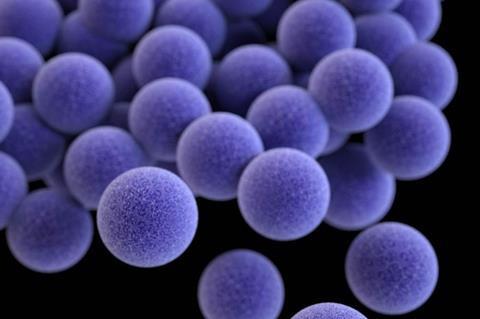
Their study revealed how two proteins enable the methicillin-resistant Staphylococcus aureus (MRSA) bacterium to secrete the toxins that make people sick. The research suggests that therapies targeting these two proteins could disable MRSA, making it less deadly and possibly even harmless. Such an approach would also reduce the risk of promoting antibiotic resistance.
The paper, which was published in the Proceedings of the National Academy of Science, suggests that similar mechanisms may exist in other bacteria, pointing to the potential for a new approach to treating other bacterial infections.
“We were looking for an alternative way of approaching MRSA,” said Seth Dickey, an assistant professor in the UMD Department of Veterinary Medicine and lead author of the study. “We were interested in understanding how the bacterium causes disease to see if we could interfere directly with the virulence factors that the bug produces. If we can disarm it, then we may not have to worry about it evading antimicrobial agents.”
Selective breeding
Antimicrobial resistance develops when a drug treatment knocks down some, but not all of the bacterial cells. The bacteria that remains tends to have some natural resistance, so if they have a chance to recolonize, the next infection will be stronger in the face of antibiotics. This unintentional selective breeding has led to super-bugs like MRSA and multi-drug resistant tuberculosis.
An approach to treating infection that makes it less harmful without killing it could eliminate the potential for such selective breeding. In MRSA, that effort has been hindered by the fact that the bacterium makes several types of toxins in abundance. Understanding each mechanism and shutting it down is tremendously challenging. So, Dickey and his colleagues decided not to look at how the cells produce toxins, but how they secrete those toxins into their host.
Previous work by Dickey and other teams found that two proteins serve as ferries to transport the molecules of toxin across the bacterial cell membrane to the outside environment. But it was unclear why there were two transporter proteins and how they functioned. Without this understanding, scientists cannot develop therapies to prevent the secretion of toxins.
Transporter proteins
To understand the mechanism at play, Dickey and his team removed each type of transporter through genetic engineering and observed how MRSA cells secreted toxins. They discovered that one transporter protein collects hydrophilic, or water-loving, toxins floating in the cell’s cytoplasm and shuttles them through the cell membrane. When that transporter was absent, hydrophilic toxins continued to build up inside the MRSA cells where they are harmless to both MRSA and any potential host.
When the team removed the second transporter protein, hydrophobic or water repulsed toxins built up in the cell. This is significant, because these toxins tend to move on their own out of the watery cytoplasm and lodge themselves in the more oily cell membrane where MRSA toxins do their damage, to host cells and to MRSA cells. So, without the second transporter protein, MRSA cells are damaged by their own hydrophobic toxins.
This suggests that future therapeutics targeting one transporter could reduce virulence, and therapeutics targeting the second transporter could reduce virulence while also having an antibiotic effect.
The study’s findings have implications beyond MRSA. When the researchers looked at the genomes of a variety of other bacteria, they found that many have genes for producing a dual transport protein system similar to the one they found in MRS






No comments yet