A review from WHO on the number of new antibiotics currently in the pipeline shows that just 12 new antibiotics have entered the market in the five years from 2017-21.
The report warns that there are far too few - just 27 - under development in clinical trials against pathogens considered critical* by WHO such as Acinetobacter baumannii and Pseudomonas aeruginosa.
Of these 27, only six are considered ‘innovative’ enough to be capable of overcoming antibiotic resistance using WHO criteria, with only two of those six targeting highly-drug resistant forms of these microbes.
Antibiotic landscape
This update on the state of the antibiotic landscape is being presented to a special online session of the European Congress of Clinical Microbiology & Infectious Diseases (ECCMID 2023, Copenhagen, 15-18 April) and is delivered by Dr Valeria Gigante, Team Lead in WHO’s Antimicrobial Resistance Division, Geneva, Switzerland.
“In the five years covered by this report, we have had just 12 antibiotics approved, with only one of these – Cefiderocol– able to target all the pathogens deemed critical by WHO,” explains Dr Gigante.
“And there are only 27 more currently under development in phase 1 to 3 clinical trials, with little innovation. Only four of the 27 have new mechanisms of action, and most are not new drug classes, but evolution of existing classes.”
Currently, one antibiotic, Solithroymcin - to be used to treat community acquired pneumonia and other infections - is at the ‘new drug application’ stage (passed through clinical trials and awaiting market authorisation) and a further seven products are in phase 3 trials having their efficacy assessed.
Dr Gigante explains that, since failures are possible even in phase 3 trials, it is difficult to predict if and when a market authorisation will be granted for these drugs.
Burden of resistance
According to recent estimates almost 5 million deaths are already associated each year due to antimicrobial resistance (AMR). However, the true burden of resistance could be even greater. Furthermore, AMR disproportionately affects poor individuals who have little access to second line, more expensive antibiotics that could work when first-line drugs fail.
Antimicrobials are not as lucrative a prospect as other treatments for pharmaceutical companies, because they are mostly short-term treatments and antibiotic stewardship programmes are aimed at conserving or ‘saving’ any such new drugs until they are desperately needed.
And they are just as likely to fail during the research and development process as any other drug for other conditions, yet offer a fraction of the revenue returns compared with, for example, cancer and cardiology drugs.
As a result of these and other factors, the research and development process for new antibiotics is challenging and poorly funded. The last novel antibiotic class was discovered in the 1980s, and the first antibiotic from this class, daptomycin, reached the market in 2003.
Resistance to antimicrobials develops because of overuse and improper use, such as people not completing their full course of antibiotics or because of the wrong antibiotic being prescribed – or, in some countries, antibiotics being used widely without prescriptions.
The global trend of inappropriate use of antibiotics is demonstrated by the time it takes for resistance to develop to new antibiotics - for antibiotics launched between 1930 and 1950 the average time to develop resistance was 11 years; for antibiotics launched between the 1970 to 2000 it was just 2-3 years.
Silent pandemic
This silent pandemic of antibiotic resistance continues to grow worldwide. Experts repeatedly warn of a ‘doomsday scenario’ in which routine medical procedures – for example antibiotic prophylaxis in cancer or other disease care – would no longer be effective, and untold numbers of people could die from what were previously simple, treatable infections.
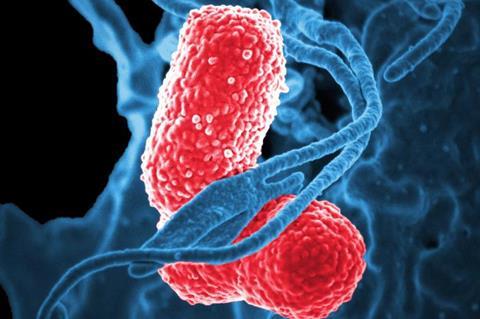
One example of a drug-resistance mechanism experts are worried about is New Delhi metallo-beta-lactamase 1 (NDM-1). Bacteria which contain the gene to produce this enzyme can break down (and are therefore resistant to) a wide-range of carbapenem antibiotics – considered part of the last line of defence in antibiotic treatments where other antimicrobials have failed.
The most common bacteria that make this enzyme are Escherichia coli and Klebsiella pneumoniae, but the gene for NDM-1 can spread from one strain of bacteria to another. Prevalence of NDM-1 containing bacteria continues to grow worldwide.
No silver bullets
Dr Gigante says: “There is a major gap regarding products addressing multi-drug resistant (MDR) pathogens such as Acinetobacter baumannii and Pseudomonas aeruginosa (just one agent authorised against all the critical pathogens and few in the pipeline). Very few agents target metallo-β-lactamases, which continue to grow in prevalence. Few new innovative antibiotics are expected in the coming years. We have no silver bullets.
”The rapid increase of multidrug-resistant infections worldwide is concerning. Time is running out for us to bring new antibiotics to market and combat this urgent threat to public health. Without immediate action, we risk returning to a pre-antibiotic era where common infections become deadly.”
She concludes: “While we face significant challenges in the fight against antimicrobial resistance, research and development efforts are underway to discover and develop new and hopefully innovative antimicrobial agents, and we have seen promising results in recent years. With increased investment and collaboration across sectors, we can make progress in the fight against antimicrobial resistance and ensure that patients have an equitable and global access to effective treatments for drug-resistant bacterial infections.”
Post-antibiotic era
In the second presentation at this session, Professor Venkatasubramanian Ramasubramanian, President of the Clinical Infectious Diseases Society of India and Consultant Infectious Diseases & Tropical Medicine, Apollo Hospitals, based in Chennai, India, asks if the current antibiotic pipeline is enough to address the needs of countries with a high burden of drug-resistant infections.
He says: “We have arrived in the post-antibiotic era. The current antibacterial pipeline is woefully insufficient to make a difference in tackling the ongoing threat of antibiotic resistance.”
He will highlight challenges in innovation including the withdrawal of large companies from the antibacterial research space, commercial failures of smaller biotechnology companies, lack of effective policy and regulatory solutions, poor return of investments, cheap generics and fluctuations in waves of infectivity.
He says: “We lack a sustainable economic model for anti-bacterial innovation. To exacerbate the issue, the current products under evaluation mainly cater to the requirements of the developed nations, resulting in a mismatch, especially in developing countries with a high burden of resistance.”
Priority pathogen lists
Prof Ramasubramanian will highlight the discrepancy in the priority pathogen list between WHO and the US Centers for Disease Control and Prevention.
He says: “This incongruity is magnified in the list of certain countries like India, who have a high burden of drug resistant organisms. A further twist to the story is when new molecules are developed for resistant organisms, that have shown promise during the developmental stage, fail to perform when strains unique to certain countries are tested. This is due to newer mechanisms of resistance that seem to be continually evolving in high burden countries.”
The talk will conclude with some possible solutions to tackle the current crisis – including the streamlining and fast-tracking of clinical trials assessing new antimicrobials; public-private partnerships across the short, medium and long-term, more investment in basic science research that underpins antibiotic development, and other financial incentives including tax breaks and better reimbursement models from national health agencies.
Topics
- Acinetobacter baumannii
- AMR in the Environment
- Antibiotics
- Antimicrobial Resistance
- Apollo Hospitals
- Bacteria
- Clinical Infectious Diseases Society of India
- Economic Equality
- Escherichia coli and
- European Congress of Clinical Microbiology & Infectious Diseases
- Industry News
- Klebsiella pneumoniae
- New Delhi metallo-beta-lactamase 1
- One Health
- Pseudomonas aeruginosa
- US Centers for Disease Control and Prevention
- Valeria Gigante
- Venkatasubramanian Ramasubramanian
- WHO priority pathogen







No comments yet