An unusual therapy developed at The Jackson Laboratory (JAX) could change the way the world fights influenza, one of the deadliest infectious diseases. In a new study in Science Advances, researchers report that a cocktail of antibodies protected mice—including those with weakened immune systems—from nearly every strain of influenza tested, including avian and swine variants that pose pandemic threats.
Unlike current FDA-approved flu treatments, which target viral enzymes and can quickly become useless as the virus mutates, this therapy did not allow viral escape, even after a month of repeated exposure in animals. That difference could prove crucial in future outbreaks, when survival often depends on how quickly and effectively doctors can deploy treatments and vaccine development will take about six months.
“This is the first time we’ve seen such broad and lasting protection against flu in a living system,” said Silke Paust, an immunologist at JAX and senior author of the study. “Even when we gave the therapy days after infection most of the treated mice survived.”
Non-neutralizing antibodies
The insights challenge a long-held belief that for antibodies to be useful as a therapy against viruses they must be “neutralizing” antibodies that bind directly to viruses and block them from infecting cells. Instead, the team engineered “non-neutralizing” antibodies, which don’t prevent infection but tag infected lung cells and recruit the body’s immune system to clear the infection. This new approach could reshape how scientists design treatments for other viruses.
“The majority of antibodies our bodies make are non-neutralizing, but medicine has largely ignored them,” Paust explained. “We show they can be lifesaving. Even with lethal strains like H5 and H7 avian flu, this therapy saved lives long after infection had taken hold.”
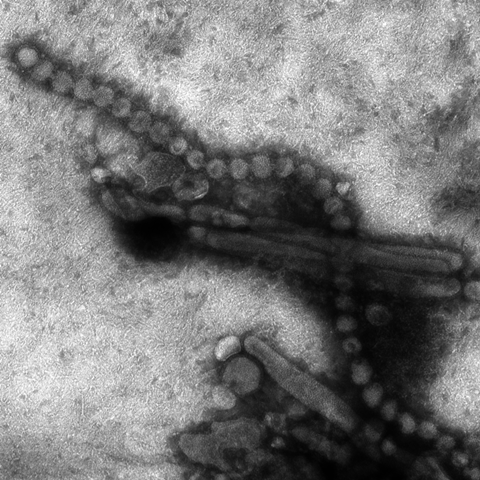
The team focused on a small, highly conserved region of the influenza A virus’s Matrix Protein 2, called M2e. This part of the virus is essential for its life cycle and remains nearly unchanged across infected cells in all flu strains, including human, avian, and swine variants.
Repeated exposure
The therapy did not lead to viral resistance even after repeated exposure, and sequencing confirmed no mutations in the virus’s M2 region after 24 days of treatment. While the team tested the efficacy of the three antibodies individually, the success came from combining them, as this approach reduces the virus’ chances of escaping three different antibodies.
“The virus didn’t mutate away even when using individual antibodies,” Paust said. “But in a flu season with millions of people taking this therapy, I would be much more confident that we can prevent escape from the therapy if we use the cocktail.”
Paust and her team found that the antibodies were effective at low doses, both before and after influenza infection. The cocktail significantly reduced disease severity and viral load in lungs, and improved survival rates in both healthy and immunocompromised mice.
One dose
When testing H7N9, a type of bird flu that can be deadly to both animals and people, the team found that just one dose of the treatment reduced the amount of virus in the lungs, even when it was given four days after infection. The reduced viral loads correlated with better survival rates. All mice survived when treated with the antibody cocktail on the first three days after infection, while 70% and 60% survived on days four and five, respectively.
“We can use very low doses, which is also promising because potential therapies could be cheaper and less likely to produce adverse side effects in people,” Paust said.
While the results are preliminary, they are promising for a future where patients could have access to stockpiled therapeutics to be deployed rapidly to fight seasonal outbreaks or pandemics. Currently, flu vaccines are updated seasonally because the virus continuously mutates, making immunity to prior strains irrelevant.
“We need something that is off the shelf when we don’t necessarily have the time to make a new vaccine if we do have an outbreak or pandemic where lethality is high, so this type of therapy could be readily available for anyone in any situation,” Paust said.
Humanized antibody
The team is working on designing antibodies for clinical trials. The idea is to make a “humanized” antibody with the same specificity to target the M2 protein, but without triggering an immune response against the therapy itself or diminishing its efficacy in humans. The team envisions a future where the cocktail could work as a standalone prophylactic for elderly, immunocompromised, and other high-risk groups, in addition to serving as a therapy for those severely ill with flu.
Other authors are Teha Kim of The Jackson Laboratory; Lynn Bimler and Amber Y. Song of Baylor College of Medicine; Sydney L. Ronzulli, Scott K. Johnson, Cheryl A. Jones, and S. Mark Tompkins of the Center for Influenza Disease & Emergence Research and the Center for Vaccines and Immunology, University of Georgia.
This research was supported by The Albert and Margaret Alkek Foundation, the National Institutes of Health (grant R01AI130065), and the National Institute of General Medical Sciences of the National Institutes of Health (grant AI053831).







No comments yet