Current standards for testing wound dressings do not work for biofilms, particularly in the case of polymicrobial biofilms, a new study has found.
Testing of wound dressings is predominantly carried out on single species of microbes in isolation, even though the wound sterile environment is not sterile and is often made up of multiple species, the University of Nottingham study revealed.
The paper, ‘Development, characterisation and evaluation of a simple polymicrobial colony biofilm model for testing of antimicrobial wound dressings’ has been accepted for publication in the Journal of Applied Microbiology, an Applied Microbiology International publication.
Global economic impact
“There is a global economic impact of over $281 billion caused by biofilms in wounds, with many patients receiving multiple wound dressings prescribed until resolution of infection,” said corresponding author Dr Shaun Robertson of the National Biofilms Innovation Centre at the university.
“In wounds, microbes are generally found as biofilms yet current standards for claims of antimicrobial activity of a dressing are performed using free living microbes (planktonic).
“The wound environment is not sterile and is often comprised of multiple species yet testing is predominantly performed using single species in isolation. We therefore tested wound dressings in a simple high-throughput model that used polymicrobial biofilms.”
Wound dressings
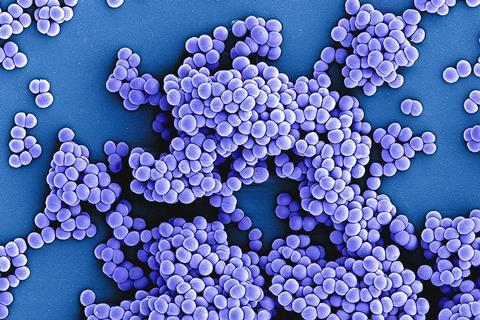
The researchers selected commercially available wound dressings as representative ones used for clinical treatment (three silver and one iodine), and began by testing the antimicrobial claims to the claimed standard which showed antimicrobial activity versus the Pseudomonas aeruginosa (Gram-negative), Staphylococcus aureus (Gram-positive) and Candida albicans (fungi) as single species free living (planktonic) and when combined together as free living populations.
They then transitioned to a colony biofilm model, proving that it had the hallmarks of a biofilm, namely production of extracellular matrix and a biofilm architecture. This was done using a combination of confocal laser scanning microscopy and electron microscopy.
Having demonstrated colony biofilms were formed, the team then tested the four wound dressings which resulted in all three silver dressings being shown to have no activity versus all three species of microbes, while the iodine containing dressing was active versus all species.
Debridement of wound
The researchers then simulated a real world aspect of wound treatment in which debridement of the wound was performed. This was done by harvesting and disrupting the colony biofilm, applying it to the wound dressings and then placing it back upon the growth agar. This showed some partial activity of silver wound dressings but this was nowhere near the same level of the antimicrobial standards claim. The iodine dressing again showed excellent activity killing all microbes in combination.
“We expected the silver wound dressings to have little to no active versus a whole colony biofilm due to how the silver wound dressings function by drawing in wound exudate, yet we expected a lot more activity when we disrupted the colony biofilm to simulate debridement. Yet that was not the case,” Dr Robertson said.
Better biofilm standards needed
“This study highlighted the need for better biofilm standards for wound dressing claims. It is clear that in this model of testing silver wound dressings were generally ineffective versus the debridement simulated model. While an in vitro study this could have implications for treatment in clinics.
“To build on these findings, we would need to perform comparative studies with other wound models and including other microbial species under different oxygenation conditions. To add additional clinical inference, testing should also be done using clinical wound isolates of bacteria and fungi to demonstrate if the findings using laboratory strains translate to the clinical strains.”
The study was led by Dr Shaun N Robertson, Dr Petra L Kohler Riedi, and Professor Miguel Cámara. This study was supported with funding from the National Biofilms Innovation Centre (NBIC) which is an Innovation and Knowledge Centre funded by the Biotechnology and Biological Sciences Research Council (BBSRC), Innovate UK (IUK) and Hartree Centre (Award Numbers BB/R012415/1 and 554 BB/X002950/1) and 3M. Manuel Romero was also supported by the Maria Zambrano program from the Spanish Ministry of Universities.
‘Development, characterisation and evaluation of a simple polymicrobial colony biofilm model for testing of antimicrobial wound dressings’ appeared in the Journal of Applied Microbiology.
Topics
- Applied Microbiology International
- Bacteria
- Biofilms
- Candida albicans
- Community
- Infection Prevention & Control
- Medical Microbiology
- Miguel Cámara
- One Health
- Petra L Kohler Riedi
- polymicrobial
- Pseudomonas aeruginosa
- Research News
- Shaun Robertson
- silver wound dressings
- Staphylococcus aureus
- UK & Rest of Europe
- University of Nottingham
- wound dressing






No comments yet