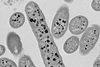
The therapeutic potential of bacteriophages (or ‘phages’) has been widely dismissed for decades in the West, despite being regularly used to treat patients worldwide in the early and mid-20th century. Recently, prompted by the escalating concern of antimicrobial resistance (AMR) and the circulation of compelling anecdotal evidence for the potential of phage therapy, global interest in phage-based medicines has skyrocketed. In several Eastern countries, however, medicinal phage practices seemingly never stopped. Many citizens of European and American countries have struggled to access life-changing or life-saving medicines from Eastern clinics (like the Eliava Institute in Tbilisi, Georgia), often fighting not only antibiotic-resistant infections, but modern legislature and prohibitive clinical regulations. Where did this divide come from? The history of bacteriophage therapy exemplifies how economic infrastructure and political attitudes profoundly influence the development of science and technology through time.
Cultural speciation
The ‘iron curtain’ that existed throughout the Cold War (1945 to 1991) presented a communication barrier between the US and USSR that, coupled with their contrasting economic systems, promoted the divergence of two independent scientific timelines. American capitalism and Soviet socialism underscored distinct niches for ideological evolution, with different ‘selection pressures’ guiding which technologies, medicines, or products were likely to succeed. Following their industrialisation in the 1940s, antibiotics could be mass-manufactured by drug companies in the US, with the growing profits reinvested in further research and development, to generate a seemingly endless cycle of innovation and prosperity. In stark contrast, the Soviet penicillin-equivalent ‘Krustozin’ was failing, and with access to Western technologies strictly prohibited, the Soviet socialist model meant the state couldn’t afford to continue investing in antibiotic research. The Soviet focus turned to streamlining the mass production of phage-based treatments for public and military use. Phages - abundant in the environment and able to replicate exponentially with minimal resources - were far more economically efficient. However, under capitalism, these intuitively positive traits become detrimental, as their natural origin makes them unpatentable and inhibits price-fixing.
A number of other key factors saw phage-based medicines commercially outcompeted by antibiotics in countries outside of the USSR throughout the mid-century, such as the broad action of antibiotics far surpassing the species/strain specificity of phages, and the comparative ease with which they could be marketed due to their synthetic (hence patentable) nature. Despite early warnings of penicillin resistance from Fleming himself, antibiotics were distributed en masse by drug companies for astronomical profits and administered with little to no discretion. The average lag between a novel antibiotic reaching the market and reports of resistant bacteria emerging is 6 years. Initially, it seemed there would always be new antibiotics available to counter these strains, but no new classes of antibiotics have been discovered since the 1980s. The capitalist model may have accelerated certain innovations, but industrial focus on short-term profit promotes homogeneity and disregard for sustainability.

Regional contexts and the reception of phage therapy
Some of the early tarnishes to the reputation of therapeutic phages were the false claims made by pharmaceutical companies in the mid-20th century when advertising supposedly phage-based products. Hunger to make quick money from international hype led to the marketing of bogus phage medicines that claimed to treat an impossibly wide range of diseases, or sometimes even allergic, genetic, and viral conditions like hives, eczema, and herpes. Combined with the ‘red taint’ of communism, the enduring stigma meant that indicating support for phage therapy could end a scientist’s career, or tank a research proposal, as recently as the past couple of decades. Another major factor underlying anti-phage stigma was the reductionist attitude of Western medicine and the instinctive rejection of natural or holistic remedies. This philosophy can be traced to the influence of JD Rockefeller (an extremely wealthy oil tycoon) in the early 20th century, whose monumental investments allowed him to shape the principles of medical science in the US. With the emergence of Rockefellers’ institutions, natural remedies were sidelined in favour of drugs with synthetic (often petrochemical) origins.
In contrast, the Soviet understanding of human health placed far greater importance on microbial ecology, informed by the ideas of early Russian microbiologists Mechnikov (who emphasised the role of the microbiome in human health) and Vinogradsky (who researched microbial communities). After the Bolshevik party seized power in 1917, scientific innovation and education became central to the new Soviet state - these were key components of the communist vision. This combination of cultural and political factors led to significant interest when French scientist Felix d’Herelle published theories identifying phages as a valuable therapeutic tool, and in time, devoted institutions were established for the isolation and mass-production of phage medicines throughout the USSR. The military demand for antibacterial treatments made these institutions essential due to their industrialised production of phage preparations; furthermore, the total loss of ideological thoroughfare throughout the Cold War insulated Soviet research from the anti-phage stigma circulating west of the Iron Curtain.

Can phage therapy succeed under capitalism?
Following the end of the Cold War in 1991, a number of unsuccessful or impeded attempts to revitalise the Western market for phages can offer insights into the obstructions to innovation that stem from a for-profit economy. Conventional clinical trials intended for single-molecule drugs are unsuitable for testing the efficacy or toxicology of therapeutic phages - geographic variability and strain-specificity have historically made large-scale phage studies near impossible, and their unpredictable pharmacokinetics, largely uncharacterised genomes, and variable dosing requirements are incompatible with bureaucratic regulatory expectations. Researching new drugs is expensive, and when the primary interest of a pharmaceutical company is profit maximisation and financial efficiency, the initial difficulty of obtaining empirical evidence in support of phages makes investment very unappealing. Besides, from the perspective of many potential shareholders, the abundance of therapeutically active phages in the environment is commercially useless; synthetic derivatives of nature’s miracles must first be developed before they can be owned and sold.
Popular media plays a dominating role in the formation of public opinion, and by extension, the acceptance or rejection of new ideas and technologies. Profit incentive often results in journalism that favours inflammatory, divisive headlines intended to attract the most attention, with little interest in integrity or the consequences of misinformation. Few examples are more potent than the overexposure given to extremely tenuous evidence linking MMR vaccination with autism, and the disastrous cultural outcomes that persist internationally. Phage science is also no stranger to wilful misrepresentation. In 2006, scientists Morris and Sulakvelidze tested the waters of the FDA with an agricultural product (LystShield) that utilised phages to prevent food poisoning caused by Listeria monocytogenes. It was approved as a food additive, and shortly after came a rush of media attention reporting that ‘viruses were being sprayed on food’ and platforming the opinions of ‘experts’ with little to no relevant experience. Considering the current distrust of science under the Trump administration, and the enduring conflation of phages with communism, it’s easy to see how frenzied media coverage could quickly mark phage research as the next target of mass defunding.
Hopeful solutions exist that could help introduce phage-based medicines into widespread use, bridging the gap between a history of imposed binaries and an aspirational future in which standard practice employs a toolkit of diverse antimicrobial strategies. Compounded by economic, political, and social limitations, a model in which ‘cocktails’ of environmentally isolated phages can be used to treat resistant infections is incompatible with the development and marketing pathways standard to clinical pharmaceuticals. The number of different phages needed for the widespread treatment of even one species of pathogenic bacteria would be immense - it would be implausible to consider each phage (or combination of phages) as a unique medicine. However, there are promising adaptations and alternatives, both legal and scientific.
The recognition of ‘magistral preparations’ in Belgian regulatory law draws a distinction between ‘manufacture’ (relevant to industrial batches of licensed products) and ‘preparation’, which refers instead to small and often personalised batches prepared by a qualified pharmacist according to patient prescription. The APIs (active pharmaceutical ingredients) are either expected to adhere to a standardised monograph or alternatively, may be approved by an accredited laboratory that performs an external quality assessment. The flexibility of this system has the potential to drastically improve patient access to effective phage-based therapies that already exist, and respected phage clinics in Europe have been pushing for the ‘magistral preparations’ framework to be adopted internationally.
‘Phage model systems’ embody a different approach entirely - rather than relying on the isolation of therapeutically useful phages from the environment, well-understood phage vectors can be engineered for use as broad-spectrum antimicrobials by widening their host range with laboratory techniques. In certain respects, this technology is ideal, as it has a clear alignment with current understandings of what commercial pharmaceuticals should look like. Moreover, due to the highly focused nature of phage research over the last century, a select few model phages are already extensively characterised (thus more compatible with regulatory expectations than the genomic unknowns of environmental isolates). The potential for phage model systems is expanded by the simultaneous progression of complementary technologies, with recent research using AI to construct novel genomes for the synthesis of ΦX174 E. coli phages that show greater fitness and ability to overcome host resistance than their wild-type template.
Reflecting on a century of barriers to the advancement and accessibility of phage therapy in the West, the potential success of these new approaches may depend largely on societal factors. In an age rife with disinformation, can the true potential of clinical phage technology be communicated to a public already uneasy about scientific intervention? How might pharmaceutical giants, infamous for their huge lobbying budgets, oppose progressive regulatory changes when their financial interests apparently favour the classification of phages as classical drugs?







No comments yet