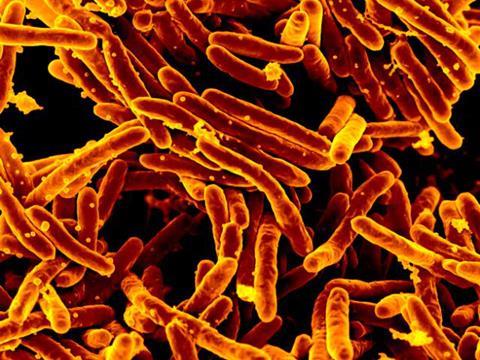
Invisible yet persistent, nontuberculous mycobacteria (NTM) quietly inhabit the world around us, found in soil, water systems, and the dust we breathe in. Once overlooked, NTM are now drawing increased attention as their infections pose significant and complex diagnostic challenges, which call for more accurate and timely identification of NTM species. Advances in diagnostic technologies offer the potential to overcome these hurdles to enable precise species-level detection, guide targeted therapy, and ultimately lead to better clinical outcomes for patients affected by these often difficult-to-treat infections.
NTMs: the emerging challenge
NTM refers to bacteria from the mycobacteria family, excluding Mycobacterium tuberculosis complex and M. leprae, the causative agents of tuberculosis (TB) and leprosy, respectively. Unlike TB and leprosy bacteria, NTM are not considered contagious and are rather picked up from the environment. NTM are frequently encountered and usually harmless; however, they can cause a range of diseases, primarily affecting the lungs. While NTM can cause health problems for people with no pre-existing conditions, they are more likely to cause serious infection in people with underlying lung disease or weakened immune systems. Studies from North America, Europe, and Asia over the last couple of decades have shown increasing incidence of NTM disease. This rising prevalence of NTM infection has been identified in a number of publications and is thought to be driven by factors including an aging population, a growing number of people who are immunocompromised, as well as improved detection and diagnosis.
Clinical relevance of key NTM species
Although over 190 species of NTM have been identified, only about 30 are considered clinically significant. Some species, such as M. szulgai, are rare but clearly pathogenic, while others, namely M. gordonae, are very common and non-pathogenic and usually not the cause of disease. Therefore, accurate identification of NTM species is crucial to ensure appropriate treatment. The official ATS/ERS/ESCMID/IDSA Clinical Practice Guidance highlights several species of concern, though prevalence can vary widely by region. M. avium complex is the most common cause of NTM pulmonary disease and can account for more than half of NTM cases in some areas. M. abscessus, notable for its rapid growth and antibiotic resistance, is frequently the second most encountered pathogen, often associated with chronic lung conditions such as cystic fibrosis and prior TB. Other pathogenic species, such as M. kansasii and M. xenopi, are less prevalent but still clinically relevant in specific populations. Different species vary in their response to treatments, which often take months to complete. Therefore, identifying the disease-causing NTM species is essential for initiation of an appropriate and effective therapy.
Treating NTM infections is challenging due to a combination of factors. While some patients are capable of clearing an NTM infection on their own without treatment, many require therapeutic help, which can include prolonged and complex treatment regimens. Certain NTM species exhibit natural resistance to antibiotics, which complicates treatment. Furthermore, managing these infections requires species-specific drug regimens, as there is no one-size-fits-all approach. Treatment typically involves the use of multiple antibiotics (often three or more) for extended periods, usually 12-24 months. For example, M. avium requires a three-drug regimen for 18 months, with success rates ranging from 45% to 70%. Moreover, even with successful initial treatment, high relapse or reinfection rates (up to 60% within 6-12 months) make long-term management particularly difficult. Better understanding of NTM disease and improvements in treatment regimens must be supported by accurate, rapid and accessible diagnostics.
Diagnostic barriers
One of the major difficulties in diagnosing NTM infections lies in distinguishing between species that represent true disease and those that are environmental contaminants. Some NTM, such as M. gordonae, are frequently isolated from clinical specimens but rarely cause disease, leading to potential overdiagnosis and unnecessary treatment. Conversely, pathogenic species like M. avium complex and M. abscessus may not necessarily cause disease, but when they do, they frequently require prompt and specific therapy. Since NTM are ubiquitous in the environment, their presence in respiratory or wound samples does not automatically confirm infection. They may end up in the lungs through accidental inhalation and show up on an NTM test, even though they usually go on to be cleared rapidly by the immune response. When NTM infections do establish, they may manifest with non-specific symptoms (cough, fatigue, weight loss, fever, etc.) which can mimic other respiratory diseases such as TB, meaning diagnosis requires both clinical and microbiological confirmation to avoid misdiagnosis. Some symptomatic infections will clear on their own, whereas others will require medical intervention. Such heterogeneity in NTM species pathogenicity and host response to infection adds enormous complexity to diagnosing true NTM infections and standardizing NTM therapy.
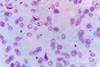
Diagnosis of NTM infection involves a combination of clinical evaluation, imaging studies such as chest X-rays, serological testing, as well as microbiological confirmation. Since symptoms vary between individuals and overlap between different NTM species and other pathogens, such as M. tuberculosis, microbiological testing is essential for definitive diagnosis. Diagnosis of NTM disease requires the collection of several samples over weekly intervals to establish that any detected NTM is the actual cause of the presented symptoms, rather than a contaminant. If the same NTM is detected on multiple occasions, and the patient is sick, then it can be assumed that this NTM is causing the disease, and therapy can be adjusted accordingly.

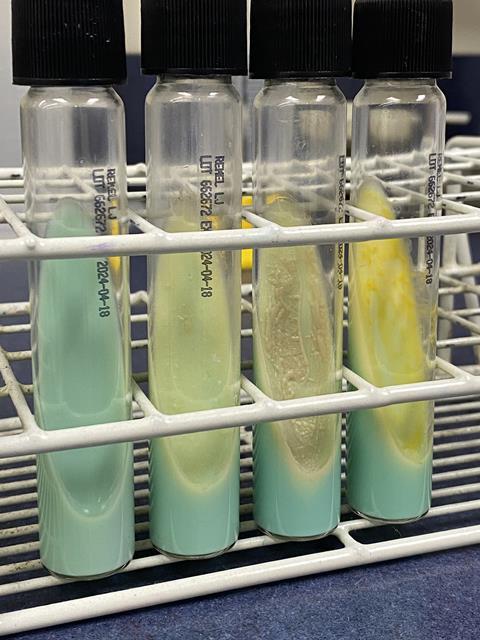
Close monitoring of patients and timely diagnostic testing are essential for optimal management of NTM infections. Traditional methods to identify NTM species usually involve a combination of solid and liquid microbiological culturing under various conditions alongside microscopy and biochemical methods to characterize growth rate, morphology, staining patterns, and antibiotic susceptibility. Although highly reliable, these techniques are slow and often delay therapeutic decisions by many weeks or months – a critical challenge when urgent intervention is needed. For example, it can take up to 2 months to identify M. kansasii using traditional methods. Without microbiological confirmation, a clinician might err on the side of caution and assume that the patient has TB and initiate a potentially ineffective or even harmful anti-TB treatment. For mild disease, with minor symptoms and minimal disease progression, a clinician would generally opt for observation in the first instance. In such cases, fast diagnosis can help the clinician confirm their decision.
The above examples emphasize the need for faster, more accurate diagnostic tools that can not only identify the NTM species but also inform clinical decision-making.
Combining the more rapid liquid culturing techniques with modern methods for DNA and protein analyses can speed up NTM identification by a few weeks. Although sequencing offers precise identification, it remains costly and not widely accessible. Alternative technologies, such as rapid molecular polymerase chain reaction (PCR) assays and matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS), are poised to transform the diagnosis and treatment of NTM infections, offering faster, more actionable results for clinicians within more meaningful timelines. For urgent cases, PCR directly from patient specimens can provide a preliminary result the same day that the patient is presented to the clinic, offering a possibility for a rapid, relevant, and often necessary intervention.
Latest developments in NTM diagnostics
Most tests used to differentiate NTM species are performed from culture. The latest molecular tests based on PCR technology can now identify the most common and clinically relevant species and are highly specific. While direct testing from sputum or other clinical specimens can avoid delays associated with culture, its current capabilities remain limited, typically detecting only at the genus level or identifying a few of the most clinically significant species. Nevertheless, direct detection of NTM from sputum and other clinical specimens can deliver results within the same day, compared to the usual wait of several weeks to months, making it a highly favorable option for urgent cases, despite the limitations. Further advancements in the field of direct testing would be a highly welcome development to improve NTM patient management.
The latest routine PCR tests help predict treatment responses in certain NTM infections. By determining the exact NTM species causing the disease, it is already possible to predict which drugs would be most effective. For example, fast-growing NTM species and slow-growing NTM species require different treatment approaches. Some PCR tests can directly determine drug resistance or differentiate between subspecies that vary in their intrinsic resistance to certain drugs, which is particularly relevant for M. abscessus subspecies. Such depth of information is crucial for guiding the clinician to the best course of therapy and offering the patient the best chance of a full recovery.
In parallel, MALDI-TOF MS developers are continuously expanding dedicated mycobacteria libraries and optimizing specialized workflows to reliably provide identification of common and rare NTM species within one hour from culture. This can prove particularly useful for recording local outbreaks of rare species and taking protective measures fast. For example, cleaning procedures of surgical equipment can be modified to include disinfectants that are effective against mycobacteria. The approach to match the clinical specimen with one of the NTM strains within the extensive NTM library offers the possibility to comprehensively identify almost any species of NTM, a feature that until now was only possible with a combination of complex culturing and sequencing techniques.
Molecular methods and MALDI-TOF MS approaches are complementary and can be selected based on the scenario. For example, PCR-based techniques can offer fast results without culture to provide early species identification and detection of resistance markers, which is critical in severe or urgent cases to enable early directed treatment. Meanwhile, culture-based MALDI-TOF MS is best placed to deliver a comprehensive species coverage, making it highly suitable for routine identification and confirmation in cases of lower time sensitivity.
Conclusion
Due to the highly complex and variable nature of NTM diseases, there are few established guidelines for the diagnosis and treatment of NTM infections. With no associated public health threat due to their non-contagious nature, there has historically been little incentive to fund large-scale research efforts, leaving gaps in data and clinical knowledge. However, as NTM infections are being recorded as increasingly common and continue to pose significant challenges, there is a growing need to undertake research to support diagnostic and therapeutic advancements.
Rapid and accurate diagnostics are critical for initiating optimal therapy as early as possible, improving outcomes for patients who endure months of uncertainty and ineffective treatment. PCR and MALDI-TOF MS technologies provide complementary advantages for microbiological confirmation of NTM infection that facilitate the wider adoption of rapid molecular and MS-based tools in clinical diagnostic laboratories. Thanks to the latest diagnostic innovations in the NTM field by forward-thinking researchers, developers, and clinicians, our understanding of NTM infections and effective treatment approaches is steadily improving. Integrated into routine testing and supported by sequencing in follow-up investigations, rapid PCR and MALDI-TOF MS approaches could significantly enhance clinical decision-making and improve patient outcomes.
About the authors
Maria Podinovskaya is a product manager at Bruker, specialising in molecular diagnostics solutions for mycobacteria. Her work focuses on supporting the development of innovative IVD tests for tuberculosis and nontuberculous mycobacteria and their implementation in clinical laboratories around the world. Prior to this, Maria’s work included the development of cutting-edge analytical tools to study host-pathogen interactions in tuberculosis and leishmania infections. Maria studied Natural Sciences at the University of Cambridge and has completed a Master’s degree in Molecular Biology of Infectious Diseases and a PhD with a focus on tuberculosis at the London School of Hygiene & Tropical Medicine.
Bernd Merkl is the Business Unit Director for Mycobacteria and TB at Bruker. With over 25 years’ experience in the diagnostic and life science industry, Bernd has occupied leadership positions at a range of companies from start-ups to larger organizations. Bernd completed a Master’s degree in Biology & Chemistry at FAU Erlangen-Nürnberg, and later a Master’s in Business Administration at the University of Regensburg.







No comments yet