Children and adolescents face greater risk of inflammatory bowel disease (IBD) when exposed to antibiotics or a Western diet at early ages, or when their family has higher socioeconomic status, according to a study being presented today at Digestive Disease Week® (DDW) 2023.

“Pediatric IBD cases are rising globally, and approximately 1 in 4 of all IBD cases are now diagnosed before age 21,” said Nisha Thacker, the study’s lead author and a gastrointestinal dietitian.
A unique concern about pediatric IBD is the impact that the inflammation has on a child’s growth and the progression of puberty, so parents should be aware of this condition and the modifiable factors that influence it.
As a part of her PhD studies, at The University of Newcastle in Australia, she conducted a meta-analysis of 36 observational studies representing approximately 6.4 million children. Thacker found that any exposure to antibiotics before age 5 was linked to a 3 times greater risk of pediatric IBD, and exposure to four or more courses of antibiotics to a 3.5 times greater risk.
Veg, siblings and pets
Lower socioeconomic status appears to be a protective factor that is associated with a 65% lower risk of childhood IBD. Greater consumption of vegetables was also protective, as was having two or more siblings, and being exposed to pets during childhood.
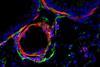
The findings that exposure to animals and having only one toilet are protective of IBD indicate that excessive hygiene can reduce microbes in the environment and interfere with development of a robust microbiome, Thacker said. Basic hygiene is recommended but allowing children to play outdoors and interact with pets in a safe environment appears to be beneficial for developing a strong immune system.
“Many of these factors can impact our gut microbiota and may have a particularly strong effect in a child,” Thacker said. “A Western diet, high in sugars and ultra-processed foods and low in vegetables, is a prime example.”
Secondhand smoke
Another risk factor is early exposure to secondhand smoke, which doubled the risk of IBD in children.
Thacker advised families with young children to emphasize a diet rich in vegetables and minimally processed whole foods, use antibiotics cautiously in early childhood, consider adopting a pet, prevent secondhand smoke exposure and avoid excessive worry about hygiene, especially in high income countries.
If a family has a history of IBD or a child has a history of eczema/rhinitis, encouraging breastfeeding, followed by a healthy diet pattern for the child, may minimize compounding effects of a Western diet on the genetic risk.
A novel risk factor identified in the study is being a non-Caucasian child living in a high-income country, which tripled pediatric IBD risk. The influence of migration on pediatric IBD is the next focus of Ms. Thacker’s research.






No comments yet