A new research paper was published in Volume 16 of Oncotarget on October 6, 2025, titled “ACTM-838, a novel systemically delivered bacterial immunotherapy that enriches in solid tumors and delivers IL-15/IL-15Rα and STING payloads to engage innate and adaptive immunity in the TME and enable a durable anti-tumor immune response.”
In this study, led by first author Kyle R. Cron and corresponding author Akshata R. Udyavar, researchers from Actym Therapeutics developed a new form of bacterial immunotherapy called ACTM-838. This treatment safely delivers immune-activating proteins directly to solid tumors. The approach may offer a new option for cancer patients whose solid tumors are resistant to current immunotherapies.
READ MORE: Tumor-targeting fluorescent bacteria illuminate cancer for precision surgery
READ MORE: Engineered bacteria paint targets on tumors for cancer-killing T cells to see
Solid tumors often suppress the immune system, making it difficult for treatments like immune checkpoint inhibitors to work effectively. ACTM-838 was designed to overcome this challenge by targeting phagocytic immune cells within the tumor microenvironment (TME). Once inside the tumor, the therapy delivers two immune-stimulating components: IL-15/IL-15Rα and a modified version of STING. Both are known to activate the body’s innate and adaptive immune responses. This combination of immune-stimulating proteins helps shift the TME from immune-suppressive to immune-permissive, enabling the body’s natural defenses to fight the cancer.
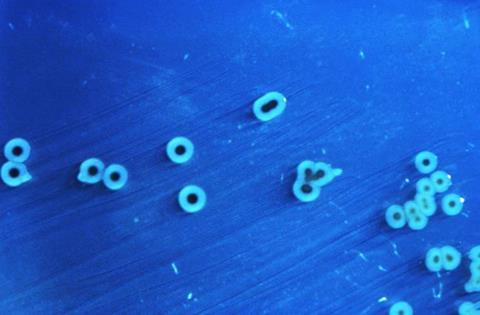
“STACT is a modular, genetically engineered live attenuated S. Typhimurium bacterial platform that enables tissue-specific localization and cell-targeted delivery of large, multiplexed payloads via systemic administration.”
Modified strain
The study highlights how ACTM-838, built on a specially modified strain of Salmonella Typhimurium, safely targets tumors and avoids healthy tissue after intravenous injection. This targeted delivery reduces the risk of side effects while ensuring the immune-boosting agents reach their intended location. Importantly, ACTM-838 also showed significantly reduced inflammatory toxicity compared to its parent bacterial strain, which had previously presented challenges in clinical use.
In preclinical tests, ACTM-838 shrank tumors and prevented their recurrence after treatment. Mice that were cured of tumors resisted re-injection with cancer cells, suggesting the development of long-lasting immune memory. The therapy also showed strong synergy with anti-PD1 drugs, a widely used class of cancer treatments, further improving outcomes in both treatment-resistant and responsive tumor models.
Changing immune cells
Researchers also found that ACTM-838 changed the composition of immune cells within the tumor. It increased beneficial cells like cytotoxic T-cells and antigen-presenting macrophages, while reducing suppressive cell types such as regulatory T-cells and exhausted T-cells. These effects were confirmed through genetic analysis and cellular studies, pointing to a broad and coordinated immune response.
This study offers proof-of-concept that live bacterial therapy can safely and effectively deliver gene-based immune modulators directly to tumors. With ACTM-838 now being tested in a Phase I clinical trial, the findings offer a new direction for cancer treatment strategies that activate the body’s own immune system, particularly in difficult-to-treat cases where other therapies fail.






No comments yet