Researchers have established the first human respiratory organoid culture system and unveiled a novel mechanism for the high transmissibility of SARS-CoV-2 Omicron variant.
A team led by Dr Zhou Jie and Professor Yuen Kwok-yung from State Key Laboratory for Emerging Infectious Diseases and the Department of Microbiology, School of Clinical Medicine, LKS Faculty of Medicine, the University of Hong Kong (HKUMed), together with Professor Hans Clevers from Hubrecht Institute, the Netherlands, a pioneer of organoid technology, and Professor Jiang Shibo from Fudan University investigated the infection and replication capacity of the Omicron BA.5 and other variants in human respiratory organoids established by the team.
The findings were published in the latest issue of Proceedings of the National Academy of Sciences of the United States of America (PNAS).
Omicron wave
The emergence of SARS-CoV-2 new variants has caused multiple waves worldwide. Omicron was first detected in South Africa in November 2021 and spread rapidly across the globe. The high transmissibility of SARS-CoV-2 Omicron variants was largely ascribed to immune escape, which led to the significantly increased risk of reinfection or breakthrough infection in vaccinated populations.
However, an important question remained unresolved, that is, whether SARS-CoV-2 has evolved to gain increased replicative fitness during the past three years and whether Omicron variants have become well-adapted in human respiratory cells. A biologically-relevant model that can faithfully simulate the human respiratory epithelium is thus needed to investigate SARS-CoV-2 infection and replication in human respiratory cells.
Organoid culture
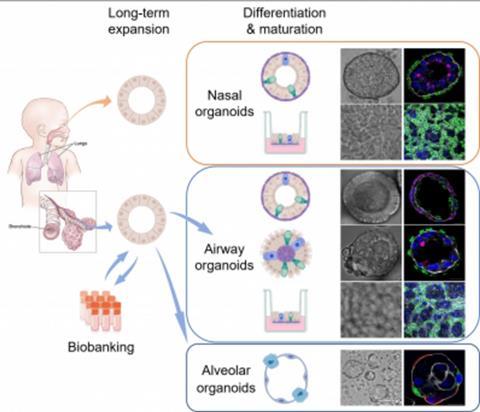
In collaboration with Professor Hans Clevers, Dr Zhou Jie and Professor Yuen Kwok-yung’s research team established the first organoid culture system of the human respiratory epithelium directly from primary lung tissues and nasal cells. These respiratory organoids were stably and consecutively expanded over half to one year.
The research team induced maturation in long-term expandable organoids and generated nasal, airway and alveolar organoids that contain all major epithelial populations in the human respiratory tract (PNAS 2018, Cell Discovery 2022, mBio 2022). The brand-new organoid culture system enabled scientists to reconstruct and expand the entire human respiratory epithelium in culture dishes with excellent efficiency and stability, representing the optimal tools for studying respiratory biology and diseases, including COVID-19.
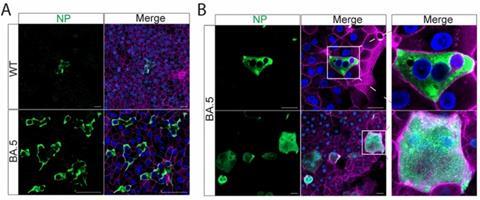
The research team then investigated the infection and replication of the ancestral strain of SARS-CoV-2 (WT), two Omicron subvariants, B.1.1.529, and BA.5 in the airway and nasal organoids, and found that BA.5 exhibited a dramatically increased infectivity and replicative capacity than B.1.1.529 and the ancestral strain WT in human nasal and airway organoids.
BA.5 robustly replicated in human nasal and airway organoids to a comparable level to an influenza virus, pandemic H1N1 (H1N1pdm). Immunostaining and confocal microscopy revealed significantly more virus positive cells in BA.5 infected nasal and airway organoids than those in the organoids infected by the other two virus stains, B.1.1.529 and WT.
Interestingly, the team observed prominent syncytium formation in BA.5-infected nasal and airway organoids, albeit elusive in WT- and B.1.1.529- infected organoids. Overall, the higher entry efficiency and fusogenic activity of BA.5 enabled viral spread through syncytium formation in the human nasal and airway epithelial cells, leading to dramatically enhanced infectivity and transmissibility.
High transmissibility
A lot of previous research has pointed out the high transmissibility of SARS-CoV-2 Omicron variants was largely ascribed to immune escape.
Dr Zhou Jie and Professor Yuen Kwok-yung’s team commented: ”Based on the investigations in the human nasal and airway organoids established by our team, BA.5 has evolved to gain higher fitness in the human respiratory cells due to the enhanced entry efficiency and fusogenic activity’. The study revealed a novel mechanism for the high transmissibility of BA.5 and provided scientific evidence for the implementation of public health policies. The respiratory organoids established by the team are robust and universal tools for studying respiratory biology and diseases.”
The collaborative research team was led by Dr Zhou Jie, Assistant Professor; Professor Yuen Kwok-yung, Chair Professor of Infectious Diseases, Department of Microbiology, School of Clinical Medicine, HKUMed; Professor Hans Clevers, Hubrecht Institute, the Netherlands; and Professor Jiang Shibo, Fudan University.
The study was conducted primarily by Dr Li Cun, Research Assistant Professor, PhD students Huang Jingjing, Yu Yifei, and Wan Zhixin at the Department of Microbiology, School of Clinical Medicine, HKUMed, who shared the first authorship. This collaborative team also included Postdoctoral Fellow Dr Chiu Man-chun, PhD candidate Liu Xiaojuan, Research Assistant Zhang Shuxin, Assistant Research Officer Cai Jianpiao, Assistant Professor Dr Chu Hin, Clinical Associate Professor Dr Jasper Chan Fuk-woo, Department Chairperson and Clinical Professor Kelvin To Kai-wang, Department of Microbiology, School of Clinical Medicine, HKUMed; together with oversea collaborators including Professor Li Gang, Nanfang Hospital, Southern Medical University; Professor Yang Zifeng, The First Affiliated Hospital of Guangzhou Medical University, Guangzhou Institute of Respiratory Health.







No comments yet