There is now one more reason to brush your teeth thoroughly every day. Korean researchers have uncovered compelling evidence that oral bacteria, once colonized in the gut, can affect neurons in the brain and potentially trigger Parkinson’s disease.
The joint research team, led by Professor Ara Koh and doctoral candidate Hyunji Park of POSTECH’s Department of Life Sciences, together with Professor Yunjong Lee and doctoral candidate Jiwon Cheon of Sungkyunkwan University School of Medicine, collaborated with Professor Han-Joon Kim of Seoul National University College of Medicine. They have identified the mechanism by which metabolites produced by oral bacteria in the gut may trigger the development of Parkinson’s disease. The findings were published online on September 5 in Nature Communications.
READ MORE: A common mouth and gut bacterium may be linked with increased stroke risk
READ MORE: Toothpaste made with salivary enzyme teams with xylitol to defeat oral microbes
Parkinson’s disease is a major neurological disorder characterized by tremors, stiffness, and slowed movement. It affects approximately 1-2% of the global population over the age of 65, making it one of the most common age-related brain diseases. Although previous studies suggested that the gut microbiota of individuals with Parkinson’s differs from that of healthy individuals, the specific microbes and metabolites have remained unclear.
Oral bacterium
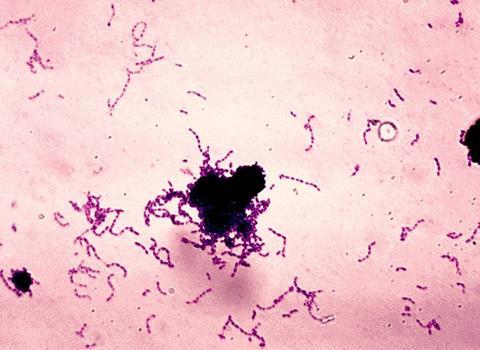
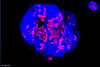
They found an increased abundance of Streptococcus mutans—a well-known oral bacterium that causes dental caries—in the gut microbiome of Parkinson’s patients. More importantly, S. mutans produces the enzyme urocanate reductase (UrdA) and its metabolite imidazole propionate (ImP), both of which were present at elevated levels in the gut and blood of patients. ImP appeared capable of entering systemic circulation, reaching the brain, and contributing to the loss of dopaminergic neurons.
Using mouse models, the researchers introduced S. mutans into the gut or engineered E. coli to express UrdA. As a result, the mice showed elevated ImP levels in blood and brain tissue, along with the hallmark features of Parkinson’s symptoms: loss of dopaminergic neurons, heightened neuroinflammation, impaired motor function, and increased aggregation of alpha-synuclein, a protein central to disease progression.
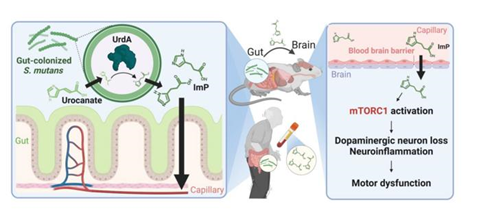
Further experiments demonstrated that these effects depend on the activation of the signaling protein complex mTORC1. Treating mice with an mTORC1 inhibitor significantly reduced neuroinflammation, neuronal loss, and alpha-synuclein aggregation, and motor dysfunction. This suggests that targeting the oral–gut microbiome and its metabolites may offer new therapeutic strategies for Parkinson’s disease.
Therapeutic strategy
“Our study provides a mechanistic understanding of how oral microbes in the gut can influence the brain and contribute to the development of Parkinson’s disease,” said Professor Ara Koh. “It highlights the potential of targeting the gut microbiota as a therapeutic strategy, offering a new direction for Parkinson’s treatment.”
The research was supported by the Samsung Research Funding & Incubation Center of Samsung Electronics, the Mid-Career Researcher Program of the Ministry of Science and ICT, the Microbiome Core Research Support Center, and the Biomedical Technology Development Program.
Topics
- Ara Koh
- Asia & Oceania
- Bacteria
- Early Career Research
- Gut Microbiome
- Gut-Brain Axis
- Han-Joon Kim
- Hyunji Park
- imidazole propionate
- Infectious Disease
- Jiwon Cheon
- One Health
- Oral Microbiome
- Parkinson’s disease
- POSTECH
- Research News
- Seoul National University
- Streptococcus mutans
- Sungkyunkwan University
- urocanate reductase
- Yunjong Lee




No comments yet