Radboudumc researchers Kirsten van Abeelen, Edwin Ardiansyah, Sofiati Dian, Vinod Kumar, Reinout van Crevel and Arjan van Laarhoven have used metabolomics to study cerebrospinal fluid (CSF) samples from tuberculous meningitis patients in Vietnam and Indonesia, with long-standing collaborators from Bandung and Jakarta (Indonesia), the Broad Institute (Boston) and the Oxford University Research Unit in Ho Chi Minh City (Vietnam).
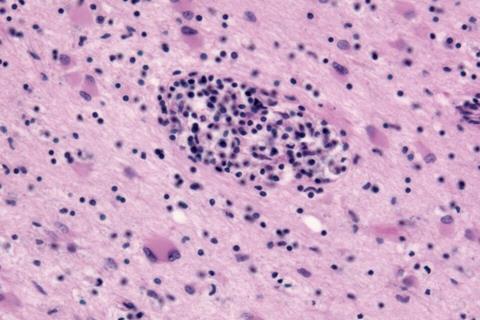
Meningitis is the most severe form of tuberculosis. Damaging inflammation contributes to its poor prognosis. Corticosteroids reduce mortality, but nearly 50% of patients still die or are left disabled.
READ MORE: Four advances that could change tuberculosis treatment
READ MORE: NIH clinical trial of tuberculous meningitis drug regimen begins
The researchers hypothesized that metabolic pathways may influence disease outcome and help develop more effective host-directed therapy. They measured levels of 469 metabolites in cerebrospinal fluid obtained from 1,067 Vietnamese and Indonesian tuberculous meningitis patients with and without HIV before the start of treatment, and observed these patients for clinical outcome.
Predicting mortality
Mortality was strongly associated with ten metabolites, including three hydroxylated fatty acids with a maximum carbon length of eight. These metabolites predicted mortality, regardless of HIV status, disease severity and cerebrospinal fluid tryptophan levels, which they previously identified as an important prognostic metabolite.
The results suggests that dysregulated β-oxidation may be an important and potentially modifiable contributor to mortality in tuberculous meningitis. Follow-up studies are underway, including quantitative trait locus mapping and rare genetic variant analysis, in the same patient groups. Future intervention studies should examine whether interventions targeting cerebral metabolism or oxygenation can improve survival of this deadly disease.
The study is published in Med.
Topics
- Arjan van Laarhoven
- Asia & Oceania
- Bacteria
- Broad Institute
- dysregulated β-oxidation
- Edwin Ardiansyah
- Immunology
- Infectious Disease
- inflammation
- Kirsten van Abeelen
- Medical Microbiology
- Metabolomics
- One Health
- Oxford University Research Unit
- Radboud University Medical Center
- Reinout van Crevel
- Research News
- Sofiati Dian
- tuberculosis
- tuberculous meningitis
- UK & Rest of Europe
- Vinod Kumar






No comments yet