Mycetoma is a chronic and progressively debilitating disease that affects thousands of people living in tropical and subtropical regions, particularly those in low-resource settings. Characterized by painful swelling, skin nodules, and pus-discharging sinuses, the condition primarily affects individuals who come into frequent contact with soil, such as agricultural and manual workers.
Despite its serious health and socioeconomic consequences, mycetoma has been largely overlooked by global medical research, resulting in limited diagnostic tools and few effective treatment options.
READ MORE: New treatment for cryptococcal meningitis enters Phase II trial
READ MORE: Mitochondrial phosphate carrier plays an important role in virulence of Candida albicans
To treat the fungal form of mycetoma, known as eumycetoma, physicians have relied on itraconazole—an antifungal medication that targets a key fungal enzyme. However, cases caused by Madurella fahalii, a lesser-known fungal species, have repeatedly shown resistance to this drug, leaving patients with few alternatives. Until recently, the reasons behind this resistance remained poorly understood.
Molecular mechanisms
In an effort to address this knowledge gap, a research team led by Associate Professor Takashi Yaguchi from the Medical Mycology Research Center, Chiba University, investigated the molecular mechanisms behind itraconazole resistance in M. fahalii.
In their latest study, published on March 27, 2025, in PLOS Neglected Tropical Diseases, the researchers used advanced genetic and biomolecular chemistry tools to uncover why this well-established treatment fails against M. fahalii but not other Madurella species.
Other members of the research team included Dr. Isato Yoshioka from the Medical Mycology Research Center, Chiba University, Prof. Ahmed Hassan Fahal from Mycetoma Research Center, University of Khartoum, Prof. Satoshi Kaneko from the School of Tropical Medicine and Global Health, Nagasaki University, and Assistant Professor Wei Cao from the Research Institute for Science and Engineering, Waseda University.
Extra gene
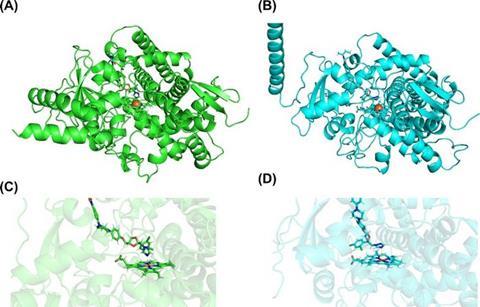
Using genome sequencing and genetic engineering techniques, the researchers identified that, unlike its treatable cousin M. mycetomatis, M. fahalii possesses an additional gene encoding the enzyme cytochrome P450 14-α sterol demethylase (CYP51). This second copy of the M. fahalii-specific gene (Mfcyp51A2), which encodes the specific target of itraconazole, has key functional and structural differences compared to the gene common with M. mycetomatis (Mfcyp51A1), effectively neutralizing the drug’s impact.
The team confirmed their discovery through multiple approaches. They demonstrated that both copies of the gene become more active when the fungus is exposed to itraconazole, with the unique Mfcyp51A2 gene showing particularly strong activation—a typical defensive response. When the researchers transplanted these genes into yeast cells for further testing, cells carrying the Mfcyp51A2 gene were markedly less susceptible to itraconazole compared to those with the standard gene version.
Binding strength
Additionally, computer simulations revealed that while itraconazole can bind to both versions of the enzyme, its interaction with the variant encoded by Mfcyp51A2 is weaker, explaining why the drug becomes less effective against M. fahalii infections. “This study represents the first report on the physiological characteristics of Madurella species using genetic engineering techniques,” remarks Dr. Yaguchi, “These findings highlight the potential of molecular techniques in uncovering drug resistance mechanisms in neglected fungal pathogens.”
Overall, this work marks an important step forward in addressing a severe disease that primarily affects impoverished communities. By understanding how drug resistance develops at the molecular level, scientists can now work on targeted approaches to overcome it, bringing hope to thousands of patients worldwide who have limited access to specialized healthcare. “Our findings will hopefully pave the way for more effective treatment strategies for eumycetoma caused by M. fahalii in the future,” concludes Dr. Yaguchi.
As mycetoma continues to pose challenges in regions with limited medical infrastructure, studies like this demonstrate the role of basic science in addressing real-world health problems. By exploring the genetic basis of treatment resistance, researchers are building the foundation for targeted, effective therapies that could benefit thousands worldwide.
Topics
- Ahmed Hassan Fahal
- Antimicrobial Resistance
- Asia & Oceania
- Chiba University
- Fungi
- Infectious Disease
- Isato Yoshioka
- itraconazole
- Madurella fahalii
- Medical Microbiology
- mycetoma
- Nagasaki University
- One Health
- Pharmaceutical Microbiology
- Research News
- Satoshi Kaneko
- Takashi Yaguchi
- University of Khartoum
- Waseda University
- Wei Cao







No comments yet