From a wartime spread of antimicrobial resistant disease in Ukraine, to superbugs in China causing “white lung” pneumonia in children, 2023 brought no shortage of new evidence that antimicrobial resistance (AMR) continues to be a pressing problem globally, and this pattern shows no sign of abating in 2024 unless a radical shift occurs.

To truly tackle the issue of AMR, York University researchers with the Global Strategy Lab (GSL) argue it needs to be understood as a socio-ecological challenge that accepts AMR as a phenomenon stemming from natural evolutionary processes. In other words, the war on bugs can’t be won; what’s needed is a major change in how people live with it.
“For the past hundred years, we’ve tried to address AMR like a medical problem. But we haven’t really made much progress in actually mitigating the deeper drivers of the issue,” says Isaac Weldon, a recent York PhD political science graduate and lead author of a new peer-reviewed article published in the prestigious Perspectives on Politics journal. “We argue that there’s a lot of potential to make progress by instead looking at it as a problem with our relationship with the microbial world and sustainability.”
Global threat
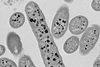
AMR stems from both the natural tendency of bacteria, viruses and fungi to evolve as well as the acceleration of that process through human interventions such as an over-reliance or misuse of antibiotics in medical settings, to the routine use of antimicrobials in the livestock industry. Global data from 2019 showed more than a million deaths a year directly related to AMR, and the COVID-19 pandemic seems to have accelerated this process.
Last year, GSL set up the AMR Policy Accelerator with $8.7 million from Wellcome Trust to deal with this urgent threat. While Weldon acknowledges that medical and technological innovation will be a crucial component in managing the issue, new antimicrobial drugs alone will not be the solution.
“What we’re currently doing is treating the symptoms and not the causes of AMR,” says Weldon, also an investigator with GSL. “Without addressing the underlying social relationships that drive our use, innovation would have to operate at an unsustainable speed as these microbes evolve faster than we can make new drugs.”
Major problems
Weldon and co-author Steven J. Hoffman, director of GSL and Dahdaleh Distinguished Chair in Global Governance & Legal Epidemiology with York’s Faculty of Health and Osgoode Hall Law School, outline major problems with the current governance approach to AMR. They introduce five principles for designing institutions for a better ecological fit of human-microbial ecosystems to minimize drug resistance:
- There’s no silver bullet. Recognizing that there is no easy fit or one-fits all solution for AMR means problem-solving must always be tailored to specific ecological situations and health challenges of diverse populations.
- Create institutions that can adapt over time. Future proofing doesn’t mean creating institutions that are strong enough to withstand change, but ones flexible enough to evolve with the changing nature of AMR and our relationship to it.
- Diversify practices. As the best way to tackle AMR is still unknown, diversifying practices can help us discover what works, when, and where.
- Create records. As practices are diversified, records need to be kept of what works to enable learning and adjustments in policy.
- Involve stakeholders. This involves everyone from the public at large, to government and decision makers.
“What we are proposing is a completely different way of looking at the issue,” says Hoffman. “We are hoping this journal article will be a foundational piece that will inspire further AMR research in this direction.”
Watch a video of Weldon explaining the research.






No comments yet