New research being presented at this year’s European Congress of Clinical Microbiology & Infectious Diseases (ECCMID) in Copenhagen, Denmark (15-18 April), highlights the devastating impact of war injuries with complex bone and soft-tissue multidrug-resistant infections suffered by 13 civilians and one soldier during the war in Ukraine, who were transferred to Germany for specialist treatment.
“Casualties of the war in Ukraine often receive suboptimal surgical and antibiotic treatment in often unsterile low resource conditions and war zone, emergency settings, sometimes for weeks or even months,” says lead author Dr Maria Virginia Dos Santos from the Charité - University Hospital in Berlin, Germany.
“The logistics of treatment in war, extensive injuries, and infections with the added challenge of polymicrobial infections, caused by various combinations of bacteria, fungi, and parasites, with multi-resistant pathogens makes these injuries extremely complex to treat.”
Transported for treatment
Since the war in the Ukraine started in February 2022, injured civilians and soldiers who were initially stabilised in Ukrainian and Polish hospitals have been transported to neighbouring countries for further treatment.
Between March and December 2022, 47 patients from Ukraine were treated in the Center for Musculoskeletal Surgery at the Charité - University Hospital in Berlin, Germany, led by the trauma and orthopaedic surgeons.
In this analysis, doctors describe treating 14 of those patients (13 civilians and one soldier) with highly complex musculoskeletal infections—six from gunshot wounds and eight from bomb and grenade explosions.
Most of the patients were male (10) and four were female, including three children. The youngest was just 14 years old and the oldest 64.
Complex damage
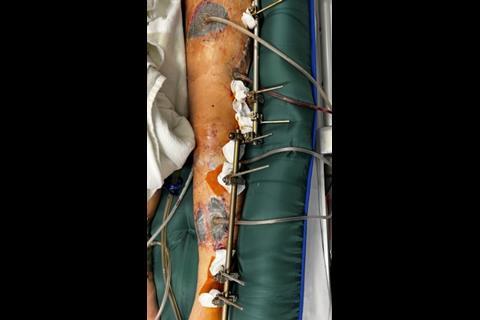
War injuries result in complex and extensive soft-tissue damage, large bone defects, contaminated by foreign objects and commonly infected with multidrug resistant bacteria.
In this analysis, doctors focus on infections of injuries with mostly multidrug-resistant pathogens, who were treated by a multidisciplinary team, requiring a combination of surgical treatment strategies and antimicrobial therapy.
Most infections were bone infections, followed by implant associated infections, soft tissue infections and septic arthritis. The most common infections were in lower extremities, but almost half of patients had more than one anatomic area affected. Two patients had multiple sites of infection.
All patients required complex anti-infective treatment strategies due to difficult-to-treat or multi-resistant bacteria, detected in tissue samples.
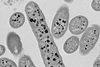
MRGN organisms
Overall,13 patients were colonised with multi-resistant gram-negative (MRGN) organisms, mainly Klebsiella pneumoniae, Pseudomonas aeruginosa, Acinetobacter baumannii, and Escherichia coli, as well as coagulase negative staphylococci, enterococci, and fungal infections.
Of the 25 gram-negative bacterial isolates identified, almost three-quarters (72%) were resistant to carbapenems and the newer cephalosporins (ceftazidime-avibactam, ceftozolane-tazobactam) – the antibiotics of last resort. And 39% of the isolates were resistant to cefiderocol, 20% to colistin, and 96% to ciprofloxacin - one of the most commonly prescribed oral antibiotics.
Empiric treatment included the combination of antibiotics colistin, meropenem and vancomycin in addition to radical surgical debridements (removal of dead [necrotic] bone and soft tissue), soft-tissue reconstructions, reconstructive surgery to stabilise and join the ends of a broken bone and joint replacement surgery, abdominal surgery, oral and maxillofacial surgery, and hardware removal, resulting in lengthy hospital stays.
Novel pathogen spectrum
“We are dealing with a completely new pathogen spectrum than what we would expect to see in Germany,” says Dr Dos Santos. “In these horrific war injuries, we are seeing high incidence of multi-resistant gram-negative pathogens, and all our cases have been polymicrobial infections. This means we’ve had to adjust our previous antibiotic treatment strategies to cover these multi-drug resistant organisms.”
As of April 2023, two patients have been discharged after treatment and are thought to have returned to Ukraine, two are currently still undergoing treatment, and another two have developed new acute infections at different sites.
The remaining eight patients have no signs of infection and have been discharged from the hospital but are undergoing an extensive rehabilitation process for their injuries, as well as the social and emotional impact of the trauma.

Topics
- Acinetobacter baumannii
- Antimicrobial Resistance
- Asia & Oceania
- Bacteria
- Charité - University Hospital
- coagulase negative staphylococci
- complex injuries
- Economic Equality
- enterococci
- Escherichia coli
- European Congress of Clinical Microbiology & Infectious Diseases
- Fungi
- Klebsiella pneumoniae
- Maria Virginia Dos Santos
- Medical Microbiology
- One Health
- Pseudomonas aeruginosa
- Research News
- UK & Rest of Europe
- Ukraine war















No comments yet