My day is characterised by its unpredictability! Medical microbiology combines laboratory-based investigations, hospital ward rounds, infection prevention, antimicrobial stewardship, and research. The unifying themes are the diagnosis, treatment, and prevention of infections, but the range of pathogens and patients are so diverse that every day is different.
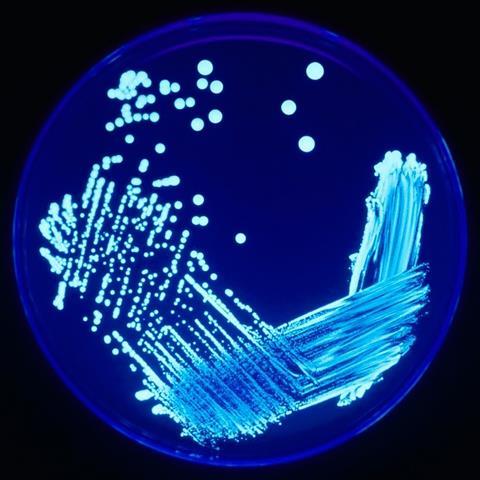
The laboratory lies at the heart of all microbiology departments. My department’s laboratory serves Leicester city, Leicestershire and Rutland, a population of over one million. Biomedical scientists and clinical scientists process specimens sent in by general practitioners as well as from University Hospitals of Leicester in-patients. Most bacteriological investigations still use agar-based culture techniques dating from the 19th century, but molecular tests such as PCR are increasing in importance. Other technologies, such as MALDI-TOF, are also transforming lab practice, making identification of bacteria far more accurate and quicker. Nevertheless, we are still some way off from the ideal of same day isolation, identification, and susceptibility testing of bacterial pathogens. My consultant colleagues and I share a daily bench round rota, reviewing interim culture results alongside patient information so we can alert ward clinicians of significant results and advise on treatment.

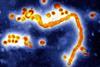
Many Leicester residents have connections with south Asia, Africa and eastern Europe, travel widely and some return with infections caused by exotic or resistant pathogens. We were one of the first laboratories in the UK to pick up a New Delhi metallo-beta-lactamase-producing Gram-negative bacterium, brought back by a patient repatriated from an Indian hospital. Other imported pathogens we encounter include the protozoal parasite Entamoeba histolytica (amoebiasis). Following several cases of serious bowel infection caused by this micro-organism we introduced a PCR test to allow us to screen diarrhoea specimens and are now discovering many more cases than we anticipated.
Hospital in-patients are highly vulnerable to infections. Invasive devices including catheters and cannulas, surgery, immunosuppression, and general debilitation caused by underlying disease increase the chances of infection. Many patients are admitted already infected or colonised with multi-drug resistant bacteria, posing a risk to others. This combination of vulnerable and infectious patients requires careful management. The hospital environment as a source of infection, such as Legionella species in water systems, is another concern. A large part of my job is to work closely with my infection prevention nurse colleagues, estates engineers and domestic services to identify and manage these risks, making sure the hospital is a safe place for patients and staff.
I also work with antimicrobial pharmacists to support the appropriate use of anti-infective drugs. Antimicrobial resistance (AMR) is a global crisis. The international spread of resistance coupled with a dearth of new antimicrobials has made the prospect of untreatable infections a reality. To tackle resistance we must drive down inappropriate antimicrobial prescribing, both in terms of absolute amount and spectrum of activity. This requires knowledge of local pathogens and resistance patterns, delivered by the microbiology laboratory, alongside infection prevention actions that minimise the number of infections that need to be treated, especially those caused by multi-resistant pathogens. Research is also important; I collaborate with academic colleagues to research behavioural aspects of antimicrobial prescribing and use of microbiological investigations, gaining insights to support stewardship.
On top of my day job, I am president of the British Society for Antimicrobial Chemotherapy, a learned society that aims to improve antimicrobial use and reduce AMR. One project we are currently developing is a global antimicrobial stewardship accreditation scheme to support better antimicrobial use internationally. I also visited Washington recently for the US premier of a BSAC-funded musical about Alexander Fleming’s discovery of penicillin and the challenge of resistance - The Mould that Changed the World – great fun!






No comments yet